By Meleni Aldridge
Executive Coordinator
On Monday 19th January 2015, I attended a Lyme Disease conference at the UK Houses of Parliament. The conference was convened by Mr Demetrios Loukas, a Lyme Disease patient himself, in order to give a voice to the concerns of the UK’s patient interest group over the NHS’ diagnosis and treatment of the vector-borne infection.
Borrelia background
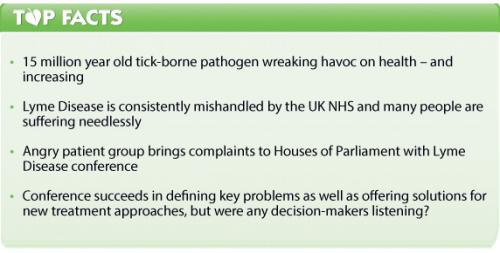
Lyme Disease is the name given to an infection caused by the pathogen Borrelia burgdorferi. Described scientifically as a novel spirochaete, it primarily lives as an extracellular pathogen and has been around awhile — 15 million years to be precise! Whilst it is now accepted there are numerous subspecies, B. burdorferi is still the only species identified in current laboratory tests. Borrelia is carried by ticks and transmitted to humans through tick bites, but only 30-40% of people are ever aware that they have been bitten or see evidence of a tick bite.
It’s acknowledged that there is a window of around 16 hours between adherence of the tick, bite and the start of transference, where the body’s defense reaction in the skin has a chance to destroy the invading spirochetes. It can take as long as 5-7 days for full transference of the infection to show, although it can take longer. The classic tell-tale sign of a tick bite infected by Borrelia is a bulls-eye rash that develops around the site of the bite or an extended expanse of redness (Erythema migrans) with no obvious cause. Here again, complications with identification arise from the fact that only 30-40% of people ever show such a rash. To complicate matters further, only 20% ever develop a feverish, summer flu-like, reaction as their immune systems wage war on the newly integrated pathogen.
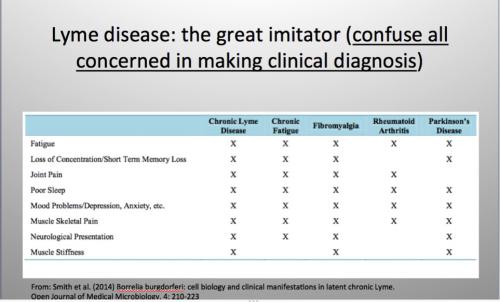
A WHO report from 2006 describes Lyme infection as the most common vector-borne disease in Europe and that it’s a multi-system disorder that can be treated with antibiotics. It’s the multi-system effect that further clouds the diagnostic lens by manifesting as disorders that can be otherwise labelled, e.g. chronic fatigue syndrome, Alzheimer’s Disease, autism, multiple sclerosis, rheumatoid arthritis, osteo arthritis, fibromyalgia, neuritis and encephalitis, to name a few.
This propensity for little or no definitive evidence of a tick-bite reaction, coupled with doctors poorly versed in recognising signs and symptoms corresponding with a Lyme infection and limited or invalid testing, has led to a large and disaffected patient group calling for an immediate overhaul of the UK’s clinical protocols.

Erythema migrans – bulls-eye rash in Lyme disease
Ticked off! Laying it on the line
The conference was hosted by The Right Honourable Simon Hughes MP and chaired by, Lady Mar. Around 15 Members of Parliament confirmed attendance, but only 2 or 3 attended and only stayed a short while. Amongst the speaker line-up was only one representative to justify the UK’s laboratory protocols for Lyme Disease from Public Health England, Dr Tim Brooks.
The opening speaker, Dr Armin Schwarzbach – an international expert on Lyme Disease and a specialist in laboratory medicine – outlined the problems with detection, diagnosis and treatment. The central tenet of his message being that government policy is far out of touch with the reality facing patients diagnosed, or awaiting diagnosis with Borrelia. The US CDC still refuses to acknowledge that persistent Lyme infection is commonplace. Preferring instead to label patients with the tag of ‘Post Treatment Lyme Disease Syndrome’ (PTLDS) if they continue to show symptoms after one cycle of treatment with antibiotics. Once labelled as PTLDS, patients are then classified as sufferers of whichever disease their symptoms best fit, with further treatment for Borrelia no longer an option. In terms of misdiagnosis, the UK is not much different.
Chris Moore, Managing Director of Nordic Laboratories, ascertained very quickly that of the 100 or so patients in the room, only around one-fifth had actually received a positive laboratory test. Yet these patients are living in the tatters of lives torn apart by the symptoms of Borrelia infection and all of them had to seek (and fund) their own treatment because nothing is available on the NHS. He made the point that times have changed. Patients are now very informed and know a lot about their own health and are looking to their doctors for support, not dismissal. After outlining the problems in detection of Borellia with current laboratory tests and introducing new technology, he illustrated the severe socio-economic repercussions of delayed or misdiagnosis with actual case studies.
Mr Loukas’ GP, Dr Mark Ashworth, gave a refreshing and humble perspective from a doctor. He admitted that he had been Demetrios’ GP for several years and during that time he had learned a lot about Demetrios, Lyme Disease and being a GP. He offered a further beacon of light when he said: “It’s so important that GPs keep an open mind and a listening ear” and that they “Had to own up to the fact that there are large tracts of medicine and huge suffering of patients that we simply can’t explain”.
Shorter commentaries followed by a selection, including doctors treating Lyme’s patients privately and the key representative of the UK’s Lyme Disease patient interest group. All agreed that there is a problem and it’s getting worse not better. Lyme Disease is on the increase and the NHS is poorly equipped to deal with it. Patients are suffering extraordinary trauma as a result, much of it unnecessarily if doctors were better educated, more extensive and valid laboratory tests were available and if NICE guidelines allowed for appropriate treatment. The latter summed up honestly by Dr Beryl Beynon, who said: “They [GPs} are no longer free to divert from NICE guidelines and their work is becoming more confined – robotic in many ways.”
Metabolic mayhem
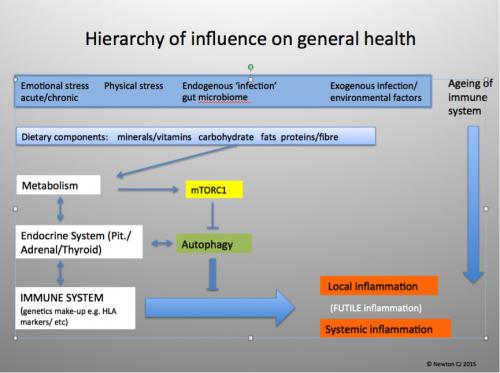
As the conference rolled on, I was left wondering when a connection would be made between the tick bite, the immune defence mechanism, chronic inflammation and metabolic dysregulation – all of which are in play with any and all of the above-mentioned diseases. I was also becoming increasingly alarmed by the inference that being in the great outdoors is dangerous, requiring public warnings about Lyme Disease and should you venture out, to ensure you cover up 1940’s safari-style. Apart from the need of as much vitamin D as we can get in the UK, getting active in nature is probably one of the most healthy choices you can make. Thankfully Chris Newton PhD, the third speaker, addressed these topics.
Dr Newton jumped straight in to elaborating how if one’s immune system is fully functioning, it’s unlikely that adhesion and transference of the Borellia spirochetes would occur if you were bitten. He showed how an immune system that has been chronically upregulated through metabolic disturbance is unable to mount adequate defence. The remedy for this being largely diet and lifestyle choices, given that poor food choices leads to chronic inflammation, as does excessive unresolved stress. He also stressed how important it was to institute these changes even as a long-term Lyme’s patient. In my opinion, his observations offered fertile foundations for future treatment and prevention protocols.
An ignominious end
During the afternoon a lot of criticism was laid at the foot of the NHS and Public Health England (PHE), but time constraints and heated emotions prevented a full right of redress by Dr Tim Brooks. Dr Brooks is Head of Clinical Services, Rare and Imported Pathogens Laboratory at Public Health England and is well known to the Lyme’s patient group. He did manage to get a few words out before the meeting broke down, and agreed that Lyme’s cases had increased considerably in recent years. However, PHE only report positive laboratory identifications and seem to feel that because England (or more correctly, Great Britain) is an island, many of the vector-borne infections on mainland Europe are not prevalent here. It was unfortunate that the conference ended without many of the patients being given a voice due to timing issues and that emotions ran high during Dr Brooks’ address. Unfortunate too that Dr Brooks lit the blue touch paper when he stated that there was an extended sequence of laboratory tests available on the NHS where Lyme Disease was suspected. The room then imploded given that not a single patient there had ever been offered such tests, which caused Lady Mar to call a halt to proceedings.
Despite the ignominious end, the conference succeeded in outlining the failure in the current approach to Lyme Disease and offering many of the solutions for a new framework. However, as with so many attempts to bridge the gap between patients and service providers, I feel that, sadly, both sides probably left this meeting no less entrenched in their own opinions as they arrived.







Comments
your voice counts
14 October 2016 at 11:36 pm
To cut a long story short I had to leave my home in 2009 because of Tick on council land. I caught Lyme Disease.
The council have taken me too court I have been find nearly £2000
for not declaring I have a home.
Even though I was put on the council list in 2010 because I could not live in my own home.
I was taken to Kettering Gen Hospital with a high temperature and blood pressure because of Lyme Disease. Kept for 3 days.
Then I was transferred to St Mary's Kettering a psychatric hospital.
and sectioned.
I was kept for 3 months.
It happened again in 2012.
My Psychatrists got their nails into me from a previous admission .
I have gone to the Health ombudsman and the legal ombudsman there is no way out.
I can't get any help.
The housing officer does not believe me.
I think this might be a test case.
I need help.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences