Content Sections
By Rob Verkerk PhD, founder, executive & scientific director, ANH-Intl
Reducing life insurance pay-outs to families who’ve lost their main income earner, or paying out less in the way of medical bills to the long-term ill, are topics that are of great interest to most insurance companies. It’s now an unassailable fact that what we eat, as well as when and how we eat, along with how we move (and think), have a huge bearing on our health, especially in our later years.
The ‘who’s who’ of nutrition
Last week, I had the pleasure of being invited, along with around 200 others, to the Centre for Global Dialogue at the Swiss Re Institute in Rüschlikon, on the west shore of Lake Zürich. The event was aptly named ‘Food for thought: the science and politics of nutrition’. Swiss Re is one of the leading global wholesale providers of insurance and reinsurance.
Find out more from John Schoonbee, chief medical officer for Swiss Re and host of the event why insurance companies are interested in nutrition.
Assembled were 200 experts from academic institutions like Tufts, Harvard, Yale and McMaster in North America, through to Oxford and Cambridge in the UK and Sydney University in Australia. Among the nutritional ‘rock stars’ present were epidemiologist Walter Willett from Harvard, cardiologist Dariush Mozaffarian and Spanish nutrition researcher José Ordovás, both from Tufts, cardiologist and epidemiologist Salim Yusuf from McMaster University in Canada, geneticist, twins and microbiome researcher Tim Spector from King’s College London, glycaemic index and load originator Jennie Brand-Miller from Sydney University, and public health physician and advisor to Public Health England Nita Forouhi from Cambridge. Each of the above, along with a number of others, gave themed presentations that followed the subject matter of a series of papers on nutrition and health that had just been published in a dedicated supplement in one of the world’s leading medical journals, the British Medical Journal. With a nod to ensure that the principles of transparent and open science were maintained, the editor-in-chief of the BMJ, medical doctor Fiona Godlee, acted as MC for the event. For those partial to social media, the event tag is #Food4Thought18.
And then there was a controversial lecture from Prof John Ioannidis from Stanford (see image below) who - frankly - laid waste to most of the epidemiology that underpinned nutritional recommendations, much to the chagrin of the likes of Profs Willett and Mozaffarian. He famously showed back in 2005 why he thought most published science was false. Referring to nutritional research, he cited factors such as poor randomisation, confounding, bias and incorrect interpretation of results by investigators as reasons for the worthlessness of the findings of many published studies. His views were bolstered by the retraction and republication from a New England Journal of Medicine analysis of the PREDIMED study just two days earlier. PREDIMED has widely been viewed as one of the most comprehensive studies supporting the Mediterranean, plant based diet.
Prof John Ioannidis (Stanford University) giving a live video presentation at the Swiss Re/BMJ conference on statistical and methodological bias in nutrition research
Given Swiss Re’s mission to get some kind of consensus on a few of the big nutrition controversies of the day, panelists had been carefully selected. Some have long been outspoken about the nature of public health policy on nutrition, especially government guidelines, such as the US MyPlate or the UK’s Eatwell guide. Among them were science and health journalist Gary Taubes, Sarah Hallberg the low carb high fat (LCHF) doctor and scientist who’s had over 3.5 million views of her TEDx talk explaining how to reverse type 2 diabetes by avoiding government ‘healthy eating’ guidelines, Nina Teischolz, author of The Big Fat Surprise, the investigative journalist who was among the first to expose the lack of evidence behind low fat public health policies, Zoë Harcombe, who did her PhD on the subject and published a meta-analysis demonstrating lack of evidence and has subsequently gone on to become an internationally-acclaimed ‘keep it real’ commentator on nutrition science, and – last but not least - British anti-sugar and processed food campaigner and consultant cardiologist Aseem Malhotra.
There were over 150 invited participants, of which I was one. They included David Unwin, aka the ‘low carb GP’ and a number of other GPs who act as medical advisors to diabetes.co.uk. Present too were patients whose stories of health transformations after going ‘low carb’ had given them Internet prominence at least. They included Amanda Atkins (no relative of Dr Atkins!)
Fall-out from the dialogue
With two packed days of dialogue, with no time even to see if the Edelweiss were in bloom, something interesting had to happen. It’s no wonder Fiona Godlee proclaimed, “There is no miracle diet, but there is a miracle meeting and this is it.”
Given the heavyweight, Big Food funded scientists present, to expect that there might be outright consensus that ‘low carb high fat (LCHF) diets’ should be the mainstay of public health recommendations might have been fanciful. But it was clear that under the firm chairmanship of Dr Godlee, nearly everyone present was open to see if some kind of consensus could be drawn out of the meeting. Consensus that might shine a few more rays of light through the often opaque and tainted science and politics surrounding nutrition.
Fiona Godlee offered her own, well-received summing-up of the meeting, captured on video along with the closing remarks by John Schoonbee, on behalf of Swiss Re.
Dr Godlee's concluding remarks about the meeting were as follows:
- Food clearly matters - we’re in crisis, and the double burden of malnutrition needs to be addressed urgently
- Evidence - we must base what is done on evidence, but a lot of the evidence is problematic, there is still good evidence available
- A mix of methodologies is needed; the scientific approach must be transparent, reproducible and independent
- Recognise the complexity of interactions within individuals and with society as a whole. Microbiome research provides a good example.
- Humility must extend to guidelines. There has been a major reversal over the demonisation of fat. Maybe we’ve reached a tipping point with our understanding that certain conditions such as obesity and type 2 diabetes can be reversed with the right kind of nutrition. If we don’t know something, let’s remain silent.
- Personalisation of approaches is essential as different people have different responses
- Prevention is key. Must move resources to prevention and to health creation. We know that disease remission (e.g. for diabetes and obesity at least) is possible.
- Food systems transformation is urgently needed, including tackling socio-economic factors
- Proper funding for research is needed. If the food industry is to be seen as the ‘bank’, we need to harness that properly. Currently there is a distortion of the food agenda because of the way vested interests operate.
But there was no formal voting system at the meeting, so Fiona Godlee's summary or the views of any other participant can't be claimed as consensus. Any view was based instead on ‘feel’ from the ensuing dialogue. That happened as much during the frequent Q&A sessions, as it did in coffee and lunch breaks. As such, just like the views that shape many of our beliefs about diet and nutrition, these views, while being informed by our different knowledge of the research, are also often experiential, anecdotal and are likely subject to uncontrolled bias.
With this admission on the table, here’s my stab at adding to Fiona Godlee's summation, focusing more on nutrition-focused issues over which there seemed to be some general agreement, even if it couldn't be formally recognised as consensus:
- food quality was more important than the relative amounts of individual macronutrients (carbs, proteins, fats) or micronutrients (vitamins, minerals, essential fatty acids, polyphenols, etc.)
- each group of macronutrients (namely fats, carbs and proteins) are far from homogeneous which means that it matters a lot what kinds of fat, what kinds of carb and what kinds of protein you eat
- eating mainly plants was better than eating too much meat, especially processed meats, and starch
- eating more veg, fruit and fibre would be good for most, but watch out for too much sugar in fruits and fruit juices and related products
- processing could damage or adversely change the characteristics of food, or not. A clearer understanding of how modern food processing techniques change food quality in relation to its health impacts is needed
- any amount of trans fats, and too much sugar and ultra-processed foods, were viewed as bad for everyone
- sweetened beverages (sodas, fizzy drinks) were among the greatest dietary sources of sugar for many people (but that doesn’t mean a sugar tax will fix the problem of excessive sugar intakes as people may move onto other sources of sugar if they find soft drinks too expensive)
- ‘low fat’ recommendations that had dominated public health policy for over 3 decades were wrong and had contributed substantially to the recent and global spiraling of obesity and type 2 diabetes
- findings from historical research may not be directly transferable to the present or future eras given the incredibly rapid changes in global food production systems and the commoditisation of the food supply
- more research was badly needed in the field of nutrition. That’s why the BMJ has added BMJ Nutrition, Prevention and Health to its journal portfolio. While randomised controlled trials (RCTs) were generally considered inappropriate tools in nutrition science, there was no consensus that traditional epidemiology that had informed most public health policy on nutrition to-date was the best way forward.
No attempt was made to try to establish what ratio of carbs, proteins and fats we should be consuming because it was deemed there are too many variables and insufficient evidence to really decide. This is in itself interesting, given these ratios are central to the existing government guidelines, which presently stipulate around 50% of energy from carbs!
On this point, I raised a question from the floor about whether it might be useful to the progress of our discussions and nutritional guidelines for the public to consider carbs as a conditionally-essential or semi-essential macronutrient, rather than an essential macronutrient. I mentioned this kind of classification is used for micronutrients, and if applied to macronutrients it would be supported by an abundance of evidence that shows we are not obligate carbohydrate consumers, while we are obligate fat and protein consumers. My question was rather quickly dismissed by Professor Dariush Mozaffarian, who proposed it was irrelevant and that we should stop thinking about macronutrient ratios and think about what foods and food groups to consume. He has his own recommendations on this (see below). See also our second story this week about our analysis of Prof Mozaffarian’s recommendations.
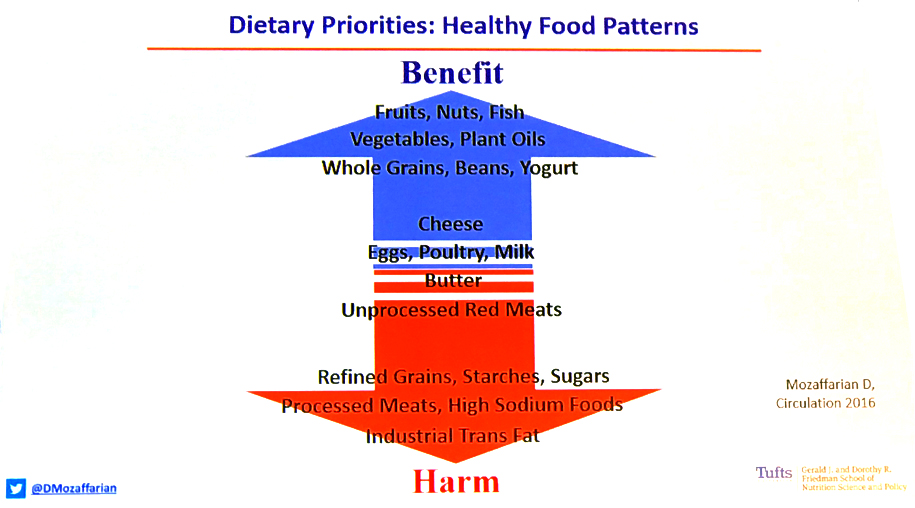
Dietary recommendations by Prof Dariush Mozaffarian, who said “eat the foods at the top in excess, the foods in the middle in moderation, and very little of the foods at the bottom”.
There was another group of issues that had strong support, but not sufficient to be considered to represent any kind of consensus.
These included:
- calorie counting was generally not very helpful for those who want to lose weight or restore metabolic health
- saturated fats are not necessarily unhealthy (sorry, Ancel Keys) and there is likely such a thing as a healthy saturated fat profile, even if it hasn’t yet been characterised
- low carb diets, which invariably were also high fat diets, were beneficial for most people, especially those with weight issues
- there was a great need for clearer definitions as to what exactly was meant by ‘low carb’ which currently may be taken to mean anything from less than 40% through to less than 5% energy from carbs, without any adequate stipulation of where these carb sources might come from or what glycaemic load they provided.
- dietary diversity especially from plant foods and plenty of dietary fibre (over 30 grams per day for adults) was key, especially to ensure the health of the gut microbiome that is in turn critical to long-term health
The barely-touched refined carbohydrate croissants on offer in the coffee breaks were testament to the widely held sentiments about low carb diets
Interestingly, some of the academics present who had advised governments to implement low fat policies that made millions become fat and die prematurely over three decades, actually admitted they had been wrong. While the international cluster of academics who had supported low fat policies – or at least hadn’t challenged them – have yet to declare a mea culpa, it was good to hear a clear admittance of previous fault from Professor Salim Yusuf from McMaster University in Canada. Being asked to explain how they got it so wrong by Fiona Godlee, Prof Yusuf said, “we were simply all drawn into believing the findings from the Seven Countries study”. This was the infamous and deeply flawed study by Ancel Keys.
Frustration
You can’t expect years of friction between different factions in the nutrition space to be resolved after two days in a secluded venue on the side of a lake in Swizerland. There was ample evidence of clear frustration among some participants, especially from clinicians, but also from scientists, myself included, who have worked closely with clinicians. Epidemiologists like Prof Darius Mozaffarian from Tufts, and Prof Walter Willett from Harvard, were understandably cemented in their view that only large, ‘high quality’ epidemiological studies would do. These, they argued, should preferably be supported by evidence from randomised controlled trials given the impossibility of banishing confounders from epidemiology. This is of course a widely held view by those espousing a classic, if not conservative, ‘evidence-based medicine’ view that suits the likes of Big Food and Big Pharma.
But what about the many assembled clinicians who had witnessed stunning results reversing metabolic diseases like obesity and type 2 diabetes among their patients once they switched to dietary patterns that were at odds with government advice? On voicing the sea change in outcomes they had witnessed since encouraging low carb, or low carb high fat (LCHF) approaches, several of these clinicians were told this was purely anecdote and it was “the worse kind of evidence” even if hundreds or thousands of patients were involved.
This is perhaps the ‘great divide’ in nutrition science. What methods should we use or rely on for future decision-making? Is an epidemiological study that might take 10 or more years to carry out with follow-up still the best and only way forward, especially given the change in dietary patterns and food quality? Should we discount patient experience or hundreds or thousands of patient experiences of positive outcomes just because we can’t fully explain exactly which factor or factors contributed and by how much?
Getting on with it
Our view is that a bottom-up, empowered approach to healthcare and self-care underpinned by individual choice is the way forward. Amanda Atkins' story below shows just what can happen when an individual is empowered and engaged in their own healthcare. Positive outcomes from multi-factorial systems among real people in real world environments are the acid test of effective ‘health creation’ (not disease management). And it’s better that we get on and do what we can, collaboratively and with dramatically improved public participation, to improve health creation. It has to beat continuing, business as usual, with the increasingly failing and over-burdened, disease-centric mainstream model, avoiding changes unless they've been demonstrated to be effective through the limited lens of evidence-based medicine before being released or recommended to the public.
Fortunately – civil society and a rapidly growing body of health professionals aren't waiting to be told what to do. We’re getting on with it. The only thing we are waiting for is the scientific community to find a better of explaining how more and more of us are getting ourselves healthier and healthier – drug-free!
A personal story, by Amanda Atkins
Amanda was a participant whose experience was dismissed as anecdotal by a leading professor of nutrition and medicine at the Swiss Re/BMJ organized ‘food for thought’ event
It was a sunny Monday in August 2016. The phone rang. My doctor barked, “Probably diabetes, blood sugar 18.4 mmol. Come in Friday to confirm with HbA1c. We will probably start you off on insulin as it's quite severe."
The previous Friday, I had my annual check-up with the usual exhortation to lose weight. I'd already lost 6kg in the last 6 weeks on my usual low fat 1200 calorie diet. I must have lost 60kg over the years on the dieting treadmill; so much effort, yet so little in the way of lasting results and now I have diabetes.
I got out my will to update it and I googled "severe diabetes". An RCT came up authored by Japanese researchers (Ed: read study here). I read it avidly. It showed me the less carbs, the better. One of the participants had reduced carbs to 11% on 1800 calories, not lost weight but reduced HbA1c from 14.4% to 5.6% in 6 months. If she could do it, so could I. I changed my diet that day.
Four days later the formal diagnosis was HbA1c 10.3% but my fasting blood sugar had already halved so I knew I was on the right track. I refused drugs and within 3 months HbA1c was 5.6% and it's currently 5.3%.
I now understand my path to recovery was inevitable. The moment I stopped putting carbohydrates in I started to get better but it generally takes 90 days of it before HbA1c hits that new healthier plateau.
I now understand it was the toxic combination of refined carbohydrates (including sugar) cooked in seed oils that caused it. I now understand I made it worse by following a "low fat, healthy whole grain, mainly plant based diet."
I now understand this was inevitable for millions when we vilified saturated fat and paved the way for "low fat inflammatory refined products".
I'm not yet as slim as I would like to be, but I am metabolically healthy. Everything else improved too, from heart, liver, kidney, blood pressure, iron, white blood cells, aspartate aminotransferase (AST), alanine aminotransferase (ALT) and gamma-glutamyl transferase (GGT). And that meant many other niggles went away too.
My new diet is a way of life, I am no longer hungry, I eat brilliant tasty foods rich in natural fats and most of all I feel on top of the world.
 Amanda Atkins – one of hundreds of thousands of n=1s: dismissed by researchers and ignored by policy-makers. Hopefully not for long!
Amanda Atkins – one of hundreds of thousands of n=1s: dismissed by researchers and ignored by policy-makers. Hopefully not for long!
Further information
Food for Thought event videos (from livestream recordings)
Food for Thought: a Swiss Re perspective
Zoë Harcombe blog on Swiss Re event
Revised ANH-Intl Food4Health guidelines
ANH-Intl Food4Health campaign page
ANH-Intl health system sustainability blueprint










Comments
your voice counts
21 June 2018 at 6:44 am
It is only a few years back that Australian Health/Government Departments were STILL showing the FOOD PYRAMID on their Internet sites.
I view with much scepticism anything that is FDA or any Government backed venture- especially in this area of our Health. In fact, If the USA FDA endorses something, then I immediately think that item is a BIG NO! this simple thinking is quite often proved overtime, as correct!
ANH Is one of the few sites/information that I have faith in & do trust, and eagerly look forward to recieving the ANH emails..
Never ceases to amaze me that all this money, education is so wasted, when the obvious is in front of these Scientists & other related bodies, and the destruction that they do to their fellow man as like sheep, they blindly follow whatever the current dictates are. Where is a questioning mindset? one queries what has happened to the Education systems, throughout the World..
When FORCED to Diagnose and very successfully self-treat, and In my never-ending health research I found official research papers of many years ago, and they gave me vital clues to put the "jigsaw" together to now have a healthy body 20-35 years younger & more - internally. Doctors cannot believe their Tests that I request, and ask me what am I doing! and make notes.
More education & money than ever, and what a stupid World we live in! where money is God. And I am truly thankful for a Californian USA food-synergised Supplement Company in this quest to return my former excellent Health.
21 June 2018 at 9:56 am
Thanks for your comment Deirdre. It's great to hear how useful the information we provide is for you and how successful you've been in improving your own health.
Wishing you well.
Warm Regards
Melissa Smith
21 June 2018 at 2:21 pm
Rob/Meleni/Melissa
This is very positive indeed. Refreshing to get the feeling that this involved healthy debate rather than the usual 'my science is right, your science is wrong' scenario. It is apparent that the message is gradually seeping through that - apart from cutting refined/ultra processed carbs, fats, meats & sugar - one size doesn't fit all when it comes to good nutrition. The personalised - suck it & see - approach is now starting to be accepted by more healthcare practitioners who have the intention of genuinely helping patients regain optimum health & wellbeing.
Another very well written article.
Thank you
Eoghan
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences