By ANH-Intl Science Unit, headed by Robert Verkerk PhD
In January 2015 we launched our ANH Food4Health Plate that provides guidelines for healthy eating for adults. This guidance is the result of evaluating typical advice from government health authorities (in the UK and USA), as well as that of independent researchers, notably those from Harvard School of Public Health. We have then taken a steer from our many years of interaction and feedback from the coalface of clinical experience, via our wide and international network of nutritional practitioners and functional medicine practitioners. The result is at odds with government advice, which we believe is still strongly influenced by commercial interests responsible for making or selling highly refined or heavily sweetened, ultra-processed foods or beverages. These types of foods and drinks have been shown to contribute to on-going, low-grade inflammation within the body, in turn a known and major trigger for chronic disease including type 2 diabetes, obesity, heart disease and cancer.
Our adult palates, as well as our trajectory of future health, is strongly affected by what and how we eat as children. In fact, early-life influences on our health stretch back to the time before we ingest our first solids, to pre-conception. Alarming statistics show that 1 in 4 kids in the UK are obese before they leave primary school, the worst rates in Europe.
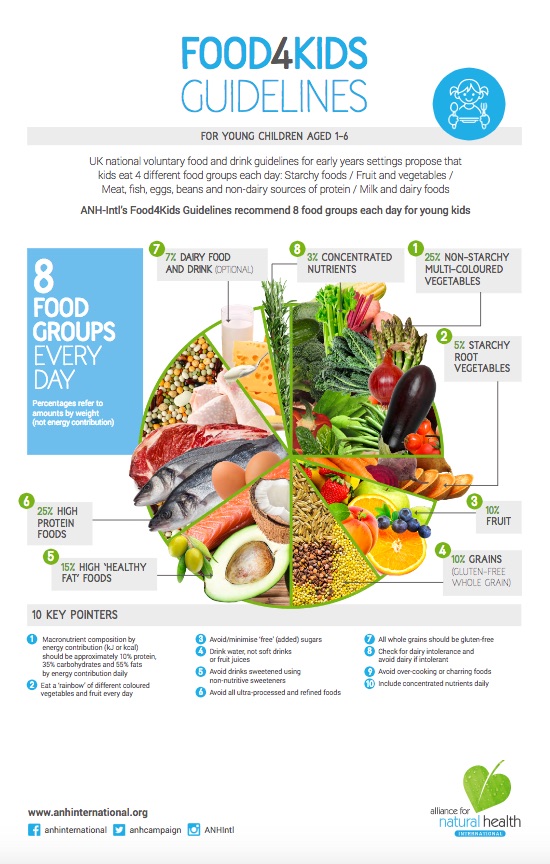
Since launching the adult Food4Health plate at the beginning of the year, we’ve had strong interest from parents asking about guidance for healthy eating for children. So, today, we launch ANH-Intl’s Food4Kids guidelines – which provides advice based both on published science, international guidance from health authorities and the benefit of experience from large numbers of nutritionists, clinicians and parents with which ANH-Intl is associated.
Variety
Kids have notoriously different interests in foods. If not diversified and nurtured, these interests can narrow to such a degree that kids end up losing out on key nutrients they need to develop and grow healthy bodies, brains, bones, muscles and nervous systems. This can happen through the impairment of cognitive function that allows us to select healthy foods, and there is now irrefutable evidence that sugary and fatty foods affect regions of the brain in such a way as to trigger addiction. This is particularly the case in times of stress, and that is why such foods have become known as ‘comfort foods’.
One of the most important roles of a parent as food provider is to help foster a broad ‘palate’ and healthy cognitive responses that ensure the child, and future adult, develops a strong interest in a diversity of foods able to deliver a wide range of nutrients to the body. Equally, it’s critical to ensure, at the same time, that addiction to unhealthy food groups, especially sugary foods, is avoided.
Variety in food choices should include:
- Colour: ensure each day that children consume ‘a rainbow’, including plant foods representing each of the six colour groups green, red, yellow, orange, blue/purple and white/tan.
- Texture: Kids should be encouraged to experiment with different textures, from crunchy (e.g. raw carrots, celery), to soft and slippery (e.g. shiitake mushrooms), to fibrous (e.g. broccoli stems), astringent (e.g. lemon, lime), sour (chard, sauerkraut)
- Flavour: Children have a natural draw to sweetness, but it’s important to develop an interest in bitter, salty, sour and umami flavours as well, whether from herbs, spices, fruits or vegetables (including fermented ones), these often being very rich sources of plant nutrients, enzymes and fibres needed to help regulate a multitude of metabolic processes within the body.
Learning about healthy eating
The Children’s Food Trust in the UK has undertaken research that shows there are many things that both parents and schools can do to help kids to develop a healthy approach to eating. These include:
- Laying the table; helping kids to develop a healthy approach to eating in the dining room, as opposed to in the lounge in front of a TV or on the move
- Empowering kids with cooking/food preparation skills
We also propose:
- Allowing kids to select foods for purchase and helping them to understand their provenance
- Encouraging kids to develop and design menus, based on healthy eating principles
It is important that healthy eating habits are developed and instilled before the age of 5 so that they become habitual and are carried into adolescence and adulthood.
How much?
We are all endowed with complex signalling systems that help to regulate the amount that we eat. The problem is that this system becomes dysfunctional if we move away from a balanced and varied diet and rely heavily for our energy requirements on fast-burning, refined carbohydrates, especially sugars. This is of course the biggest challenge for kids – given the addictive capacity of sweet foods that, for the majority of our evolution, were hard to find. Now, we can walk into a supermarket, newsagent, garage – or simply open the refrigerator – and find concentrated sources of calorific, nutrient depleted foods.
Therefore, if we provide children with a diversity of foods containing sufficient proteins and healthy fats, which are especially good at signalling satiety, along with complex carbohydrates from vegetables and fruit, children tend to regulate the amount they eat very well. They develop eating patterns that greatly reduce their risk of developing metabolic diseases like obesity and type 2 diabetes as well as tooth decay, both of which are escalating rapidly among children and adolescents.
Having said this, assuming there is an interest in counting calories, the Food and Agriculture Organization (FAO) and World Health Organization (WHO) of the United Nations agreed in 2001 levels of energy requirement (as kcal [calories] or kJ [kilojoules] per day). Refer to Tables 4.5 and 4.6 in FAO/WHO guidance, according to 3 different levels of physical activity, in which the highest level of activity is preferred for long-term health. These values vary between around 85 kcal/kg body weight per day for one-year-olds through to around 50 kcal/kg body per day for highly active 17 and 18 year-olds. For example, according to these data, the daily caloric intake for a moderately active 6 to 7-year-old is estimated at 1575kcal, while a heavily active 18-year-old it will need almost 4000 kcal daily.
Among the most comprehensive food composition and energy counter databases available are:
- USDA National Nutrient Database for Standard Reference
- UK McCance & Widdowson’s Composition of Foods Integrated Dataset (CoFID)
We would suggest, however, as advised by UK cardiologist and anti-sugar campaigner, Dr Aseem Malhotra; “It is time to stop counting calories, and time instead to promote dietary changes that substantially and rapidly reduce cardiovascular morbidity and mortality”.
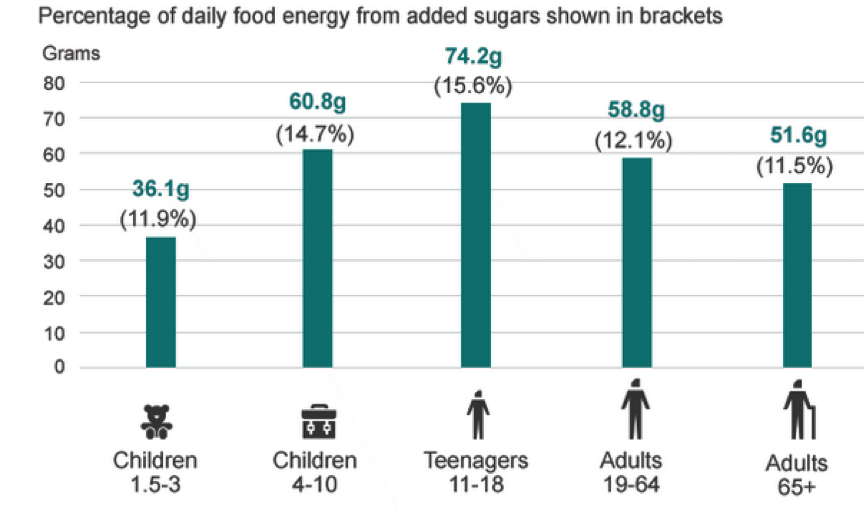
Sugar
Most kids eat far too much sugar. Kids aged 4-10 in Britain consume as much as 60 g per sugar per day, a large proportion of this being in soft drinks and cereals (Table 1). For teenagers it’s even worse, at 74 g. While some of this sugar occurs naturally in fruits and milk, much of it is added sugars – and hidden sugars in processed and ready-made foods. A single, large vanilla milk shake, for example, from Macdonalds contains a whopping 72 g of sugars. A 330 mL can of Coke contains 35 g. These high levels of sugars are not only rotting kids teeth at an unprecedented rate, they are also contributing to metabolic disease like obesity, at an ever-younger age. While Big Food is doing all it can to deny any links between sugar and addiction, there is both correlative and causative evidence of a link.
Table 1. Consumption of added sugars among different population age groups in the UK
Source: National Diet and Nutrition Survey, Rolling Programme (2008/2009 – 2011/12)
A large study has shown that for every 150 additional calories consumed as sugar, there is an 11-fold increase in rate of type 2 diabetes when compared to when these calories are derived from fat or protein.
The latest advice to the UK government, from the Scientific Committee on Nutrition, proposes that no more that added (‘free’) sugars (i.e. that which is not naturally contained in whole, unprocessed fruit, or milk) should not exceed 5% of the energy. That amounts to just 25 grams total added free sugars per day for a 2000 kcal daily energy intake, well below the 35 g in a can of regular Coke and only a fraction more than that in a Coke Life.
How often
A breastfeeding infant may typically need to feed every four hours, such is their nutritional requirement. This same feeding frequency generally continues through infancy and into childhood, although increasingly it is built around 3 main meals, breakfast, lunch and dinner, with lighter snacks in between. While this is fine, and in fact wholly appropriate, for kids who are gaining excess weight, the amount of sugars and the frequency of eating are areas that need careful review. Limiting snacks in between meals is one of the most effective ways of dealing with this issue, and ensuring that such snacks contain limited if no added sugars.
What to eat
Healthy eating advice supported by governments, such as the UK Children’s Food Trust’s 80-page voluntary guidelines, normally partitions food into groups:
1. Fruit and vegetables
2. Starchy carbohydrates
3. Meat, fish, eggs, beans and other non-dairy protein sources
4. Milk and dairy products
Government authorities recommend that typically half the energy (calories) come from carbohydrates. Our guidelines, by contrast, which are consistent with what we know of our evolutionary background, propose that only 35% of energy is derived from carbohydrates, as few of these coming from added sugars as possible, with a protein level set at around 1.2 g per kg body weight and healthy fats contributing the greatest to daily energy, at around 60%.
From 4 to 8 food groups
ANH-Intl’s Food4Kids guidelines (Figure 1) double the number of key food groups that need to be taken into account, as follows:
1. Non-starchy vegetables
2. Starchy vegetables
3. Fruit
4. Gluten-free grains
5. High animal or vegetable protein sources
6. Healthy fats
7. Milk and dairy products
8. Concentrated nutrients (e.g. fresh herbs, spices, Omega-3 essential fatty aids, vitamin D3)
The biggest challenge with balancing a child’s diet according to say the UK Eatwell plate or the US MyPlate using these food groups is the excess of refined carbohydrates and sugars that can so easily be consumed.
The 10 Food4Kids guidelines
A balanced and varied daily diet for infants, children and teenagers can be achieved using the following guidelines and adjusting amounts, portion sizes and meal frequency according to the age, size, gender, activity level, and cultural and other requirements of the child(ren):
1. Macronutrient composition of protein, carbohydrates and fats should be approximately in the order of 10%, 35% and 55% respectively of daily energy, bearing in mind fats contribute 9 kcal per gram, as compared with the 4 kcal per gram for proteins and carbohydrates (See Food4Kids graphic below). Protein levels should be maintained for children from 1 year of age through to 18 at approximately 1.2 g per kg body weight. This is around, or just over, the so-called ‘safe’ level set by the WHO which includes a conservative safety factor (excessive nitrogen from protein can modulate renal function and may in some circumstances lead to kidney disease with prolonged intakes well above these levels; more moderate, higher intakes tend to be adaptive)
2. A rainbow every day. Each day, children should consume a ‘rainbow’ of plant nutrients from whole fruit and vegetable sources, containing no added sugars, that includes all six colour groups, namely green, red, yellow, orange, blue/purple and white/tan. See Institute for Functional Medicine’s Phytonutrient Spectrum Checklist for Kids. These levels of intake will ensure that required fibre levels (which should range from around 20-40 g per day, depending on gender and age) are maintained in the diet
3. Avoid/minimise ‘free sugars. Children should not consume more than 5% of their total energy each day from ‘free sugars’, which includes all sugars except those naturally contained in whole fruits. Fruit juices are not counted as whole fruits and are a major source of sugar in the diet and so consumption should be minimised or avoided where possible. Carbonated (fizzy) beverages (soft drinks) are among the greatest contributors to sugar intake in children and should be avoided. Be mindful of hidden sugars in sauces, salad dressings, biscuits, etc.
4. Drink water, not soft drinks or fruit juices. Water needs to be consumed regularly (typically 1-2 litres daily, depending on age, weight and level of physical activity) to avoid dehydration and is best consumed away from meals to avoid dilution of enzymes in the gastrointestinal tract
5. Avoid drinks sweetened using non-nutritive sweeteners. Avoid regular consumption of intensely sweetened drinks that are either artificially sweetened (e.g. with aspartame, sucralose, acesulfame potassium, saccharin) or sweetened with natural sweeteners (e.g. steviol glycosides, polyols) as these may also induce insulin resistance and confuse our cognitive and reward behaviours
6. Avoid all ultra-processed and refined foods, especially carbohydrate-based ones or ones containing hydrogenated or trans fats. Prepare foods as far as possible from scratch using wholefood ingredients, engaging the children in the food selection, preparation, serving and tidying up process
7. Gluten-free whole grains. Where grains are consumed, these, as with the adult plate, should be gluten-free whole grains (e.g. brown rice, quinoa), given the prevalence of intolerance to gluten and the unknown status of sub-clinical intolerance among children
8. Check for dairy intolerance. If there are any suggestions of intolerance from dairy foods or drinks, all forms of dairy should be avoided. Seek advice from a nutritionist or other suitably qualified and experienced healthcare professional to establish any food intolerances and to ensure adequate substitution of nutrients. Bear in mind, lactose intolerance may develop during childhood and is common in certain ethnic (e.g. Far Eastern) groups
9. Avoid heat-damaging or charring foods as excessive heat damages proteins and some heat-sensitive healthy fats (e.g. extra virgin olive oil) and introduces harmful (potentially carcinogenic) chemicals such as heterocyclic amines and polycyclic aromatic hydrocarbons
10. Include concentrated nutrients in the form of fresh (or good quality, non-irradiated) herbs and spices, along with some supplements, which may include vegetarian protein sources (especially for vegan/vegetarian children) and a limited range of food/dietary supplements, including:
- Vitamin D3 (25 mcg [1000IU)/day, from 1 month to 18 years) except when in at least 20 minutes of 80% sunlight exposure of body surface area (without sunscreen) during summer months
- Children’s multi-vitamin/mineral (without sugar, sweeteners, fillers or artificial ingredients), as per directions
- Omega-3 oil; including EPA and at least 200 mg DHA daily (especially on days when oily fish is not eaten)
- Probiotics, from fermented foods (e.g. sauerkraut, tofu, tempeh, kimchi, etc) or good quality supplements, as per recommendation by nutritionist, other health professional or manufacturer/supplier.
Example: Healthy eating for a six-year old
We provide below a typical scenario of what a day of healthy eating according to the ANH-Intl Food4Kids guidelines might look like. For children younger, or older, amounts can be altered proportionally according to weight (see growth charts for boys and girls). It is important, especially with children, to not be too prescriptive given variations in cultures, genetics, levels of physical activity and preferences. Therefore it must be stressed that the following is simply an example of one day’s eating for a typical six-year-old girl or boy, and different foods should be consumed on different days.
Carbohydrates
- 2 cups non-starchy (e.g. mixed, coloured vegetables) (15 g carb, 60 kcal)
- 0.5 cup starchy carb grain (e.g. red quinoa, brown rice) (15 g carb, 60 kcal)
- 0.5 cup starchy root vegetable (e.g. sweet potato) (30 g carbs, 7 g sugars, 120 kcal)
- 1 medium banana (27 g carbs, 14 g sugars, 108 kcal)
- 1 apple (Granny Smith) (23 g carbs, 16 g sugars, 92 kcal)
- 1 cup raspberries (7g carbs, 3 g sugars, 28 kcal)
- 1 teaspoon maple syrup = 5 g sugars/carbs (20 kcal)
- +5 g sugars from 120 g of whole Greek yoghurt (20 kcal)Total energy from carbs = 508 kcal
Protein
- 25 g protein total, from:
- 82 g beef sirloin steak (150 kcal)
- or 84 g chicken breast (130 kcal) (= 1 small chicken breast)
- or 90 g lamb chop (150 kcal)
- or 98 g (small) fillet of wild Atlantic/Alaskan salmon (180 kcal)
- or 25 g pea protein isolate (100 kcal)
Note: the above foods should be cooked carefully and slowly using healthy fats (see below) and fresh herbs and spices
- Or partially from animal or plant sources e.g. 100 g of cooked lentils/dahl will yield around 9 g of protein together with 11 g protein from 120 g of whole milk Greek yoghurt Total energy from protein = 100 kcal
(Total energy from high protein sources = 100-180 kcal)
Fats
- Half an avocado (15g fat, 135 kcal)
- 1 tblsp nut (e.g. almond, cashew, not peanut) butter (16 g, 9 g fat) (81 kcal)
- 10 tree nuts (e.g. almonds, macadamia, cashew) (~6g fat, 54 kcal)
- Omega 3 DHA/EPA 0.6g (minimum daily intake) This may be derived from as little as 28 g of mackerel, 34g of Atlantic or farmed salmon, 38 g of tuna or 54 g of herring (but would require 200 g of cod!) (5kcal)
- Butter, preferably organic – 2 tblsp (22 g, 198 kcal)
- Extra virgin olive oil (unfiltered) – 1 tbsp (13.5 g, 120 kcal)
- Extra virgin coconut oil (odourless is available commercially) for cooking – 2 tblsp (27 g, 243 kcal)
- Whole milk, live culture Greek yoghurt, 120g serving (6 g fat) (54 kcal from fat, 116 kcal total)Total energy from fats = 890 kcal
TOTAL ENERGY INTAKE = 1498 kcal (34% from carbs, 7% from protein and 59% from fats)
TOTAL SUGARS INTAKE = 50 g, with only 5 g ‘free sugars’ (from maple syrup)
Action for adults!
We believe governments have it badly wrong and children today are victims of now discredited, 30-year-old policy and advice, based on no proper scientific evaluation, to banish fats from the diets of children and adults alike.
The Food4Kids guidelines show you how to combine and prepare foods, putting healthy fats back in the driving seat. The nutrients are incredibly important for a multitude of purposes, not only to satiate our children, but to provide energy and feed growing brains.
Please do what you can to share this information widely, as well as among your friends and local communities. We’d love to hear how you go and please check out our sister and consumer empowerment arm at Bite the Sun to find recipes that encompass many of these principles.
Go to Food4 Health campaign







Comments
your voice counts
There are currently no comments on this post.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences