Content Sections
Article update 19/06/17
As the world population blows out to nearly 10 billion by 2050, we will face two entirely different challenges. In much of the developing world, getting enough food to avoid mass starvation will be among the biggest challenges. For the Western world, it’s not population growth or food supply that will be the overriding problem. It’s healthcare and social stability given that our societies will need to deal with very large numbers of old people burdened with very high rates of sickness.
That’s unless we do something about it. Interestingly, however diverse these two sets of challenges might seem, the solution to them might be remarkably similar as we show below.
Doomsday scenarios
The Bible, Nostradamus and, more recently, the United Nations (UN), have all warned of famines and shortages of food supply. But, is there a plan to guard against it? A 1972 book called Limits to Growth predicted that our civilisation would probably collapse some time this century, and recently Australian researchers have found this prediction to be ‘spookily’ on-track' (see scenario in Figure 1).
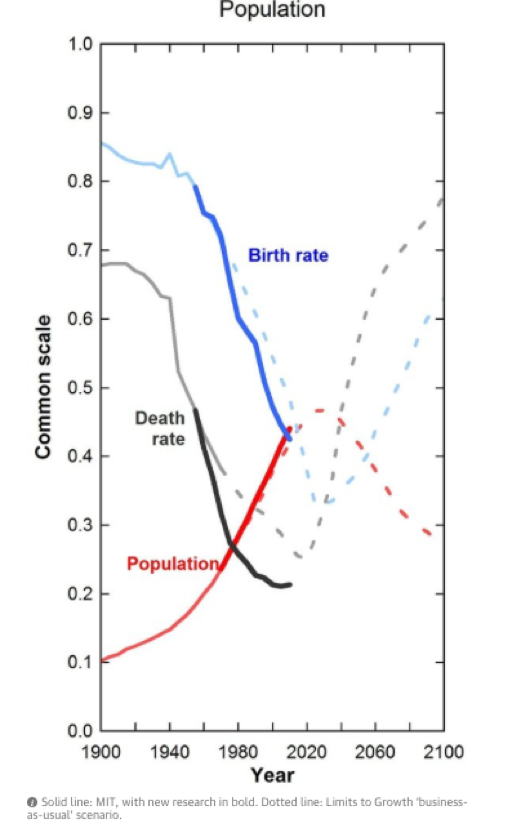
Fig 1. Limits to growth 'business as usual' scenario
The population keeps rising…….and ageing!
The global population is set to reach 9.7 billion by 2050, with Africa and Asia contributing most to that growth. Biotechnology companies would have you believe that the only way to feed the world is with GM foods.
However, this rise in population is absolutely not being mirrored across Europe and North America (Figure 2). In Europe, rather contrastingly, it is shown that a third of the population will be aged 60 or above by 2050, giving us a wholly different problem that could collapse the healthcare systems of today and cause mass social destabilisation with all its consequent issues, many being almost unthinkable.
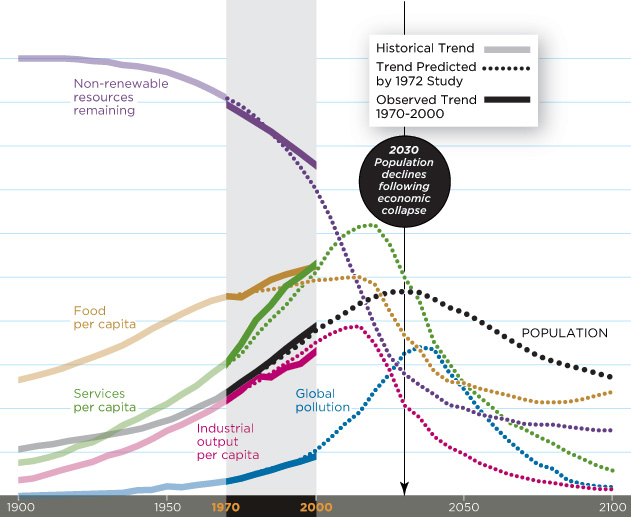
Figure 2. Projected population growth
In the UK, when the National Health Service (NHS) was founded, nearly half of the population died before the age of 65. Hospitals were there for infectious diseases, but now the non-communicable disease pandemic threatens the sustainability of that health system.
Food, diets and nutritional status are important determinants of non-communicable diseases such as obesity, cardiovascular disease, type 2 diabetes and dementia. Governments are becoming increasingly aware of their obligation to ensure that agricultural and food policies are supportive of health policies. Are they empowering citizens to take the right steps early in life so they can enjoy a long life in good health?
In the UK, with pressure from over 2000 senior NHS doctors calling for increased spending on health and social care over “unacceptable levels of safety concerns”, it is clear to see that there is much-needed change in the way that Western systems handle and distribute healthcare to society.
It’s becoming increasingly apparent that throwing more money at the present system isn’t going to achieve very much, especially when the system is based on drugs that don’t cure the very diseases that represent the main health burdens!
Such dependency on repeat-prescription Big Pharma would be a thing of the past, handing the power of choice and knowledge of individualised healthcare, once again, back to the people where it has always belonged.
Sustainability and safety of our food supply and sustainable healthcare
Unsurprisingly, the European Commission (EC) is looking closely how it might face the challenges ahead, given its remit as the ‘executive’ power of the European Union (EU), including the management of a population of over half a billion people.
We’ve digested the EC’s most recent report, “Delivering on EU Food Safety and Nutrition in 2050 - Future challenges and policy preparedness”, on the subject and found it both alarming and refreshing. This progressive report was the inspiration of the Deputy Director-General responsible for food safety, DG SANTE, Ladislav Miko PhD, who like our own executive director, Robert Verkerk PhD is a qualified ecologist.
The EC considered four possible scenarios. Some of these scenarios include functional processed food, but with added pharmaceutical substances - “phoods”.
Most scarily, the worst case scenario represents the current track we’re on. The EC calls it the ‘Global Food’ scenario as it’s based on global food corporations controlling the world food supply. The outcome? Even higher chronic disease burdens — and this leads to an inevitable collapse of our current system of healthcare – and, along with it, the entire social and economic infrastructure.
The EC’s report was particularly refreshing in its recognition for the importance of agroecological food production systems, the approach long upheld by ANH-Intl as the only sustainable approach to human food supply. It also recognizes that diet and lifestyle are the major factors impacting the health of citizens.
Moving towards healthcare sustainability
Long lives are OK if people are productive and healthy. But they are a major problem if people aren’t. In the UK (and the rest of Europe), we desperately need a fundamental shift from a healthcare system that aims to be curative to one that is preventative.
Nutrition education will ensure a reduced reliance on processed foods and simple carbohydrates, and encourage greater physical activity.
Governments must move to implementing a risk-benefit approach in regulation to avoid unjustified, disproportionate bans on healthy foods and supplements, and use scientific and legally rational thinking to communicate the health benefits of foods by commercial operators. A complete revamp of the nutrition and health claim regime in the EU using a graded system, for example, could solve the position on botanical nutrients.
A sustainable future
A sustainable society that’s not on the brink of crisis is one in which individuals in it are fully empowered with regard to their health. That doesn’t mean we don’t need doctors or health professionals. We absolutely need them, but we don’t need to be told there is only one way to manage our health — and that involves drugs or surgery. We also don’t need huge hospital waiting lists, iatrogenic (medical) errors and hugely over-stretched medical professionals that can no longer cope with health challenges that ultimately can be prevented. To take this pressure off the system we have to make dietary and lifestyle management the centre-piece of our health management system – and put its control back in the hands of the individual.
In essence, this is the sustainable healthcare scenario that’s central to ANH’s mission and vision of the future and is supported by ANH's Food4Health campaign and guidelines.
A community supported, self-empowered health system would allow people to take ownership of their health and would facilitate information sharing between all health professionals.
The future is in our hands – let’s make it happen. These concepts are the ones that are integral to all the advocacy work we’re doing to help shape a better future for us all. It’s the people’s choice.








Comments
your voice counts
01 February 2017 at 10:11 pm
The British Government was the only one which didn't support the rest of the EU in refusing the USA's GMO grains and hormone-fed meat. So after Brexit, when we stand alone, what's the betting that whether we like it or not, we'll be "accepting" the USA's output in order to get a favourable trade deal.
19 May 2017 at 11:22 am
Completely agree. Out of the EU makes us very weak.
01 February 2017 at 11:09 pm
We have to re-examine our food production techniques and try and return to a more natural state. In the book entitled "Secrets of the Soil" published in 1998, it shows how nature can be harnessed to restore over-worked land by simply improving the soil microbiome, just as we are now discovering how good health can be achieved by improving our own gut flora.
In the book, a man in California in the early 1900's was able to transform all of a city's biodegradable rubbish into a first-class soil restorer, by using a method as simple as burying fresh cattle dung in cattle horns for six months, resulting in a concentrated soil probiotic that could be diluted a thousand times and sprayed on the land. He used this concentrated bacteria to spray the biodegradable material as it entered his large storage sheds, and within days had a remarkable soil conditioner, which he sold back to farmers. The advent of artificial fertilisers soon put and end to this business.
If you go to YouTube and look for Plasma School Library Australia, you will see a totally new approach to increasing and enhancing crop yields. Lisa and Jim Mc Donald have put up a few videos showing remarkable results in the commercial growing of lettuce using this simple technology, that anyone could adopt at home. The new science is called Plasma Technology using GANS, or gas in an nano state for food production, and for health. This technology was first put forward by MT Keshe, an Iranian Nuclear Physicist, and it now has thousands of followers right across the world. Trials are on-going in curing disease such as cancer, aids and diabetes, cleaning polluted water, increasing crop yields, reducing power consumption and so on. I know it sounds like some snake oil salesman, but I have experimented with it for pain relief on many friends, and it has worked every time. The Keshe Foundation was initially formed to research space flight, but it has grown into a technology that will be our future survival. Have a look at Jim and Lisa's videos, it will give you and idea of the potential of this technology.
02 February 2017 at 12:30 pm
Dietary and lifestyle management is the way to go but people are reluctant to do this - taking a pill is an easier option. Have we forgotten what it feels like to be healthy? I think some people have. A lot of hard work for us nutritionists but we are passionate enough to succeed in spreading the message!
02 February 2017 at 11:44 pm
I was 31 before my first truly healthy day. Being healthy feels soooo good! Unfortunately, even a small amount of preprocessed food has me sick for a long time. Home cooking from scratch and certified organic. otherwise there is no escaping those health issues.
02 February 2017 at 11:36 pm
Regulating against GMOs, pesticides, preservatives, desiccants, flavor enhancers, artificial flavors, artificial sweeteners ...., Would do more for the health care system than giving it more money. There are so many things in the food produced by big food production companies. Most non-communicable diseases can be attributed to these.
To add to the list given: chronic pain, ADHD, seizure disorders, irritable bowel syndrome, Migraines, muscle spasms,....
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences