There is as yet no consensus over effective protocols for treatment or prevention of Covid-19. The search for drug-based treatments has not delivered much hope, with remdesivir’s benefits being shown to be only marginal. UK scientists are currently being hailed as heroes as they proclaim the effectiveness of a steroid, dexamethasone, for the treatment of covid-19 patients. But there is no acknowledgement of the success of the MATH+ protocol used to great effect by a group of emergency doctors in the US, which uses a steroid as part of its protocol that includes natural products such as vitamin D, vitamin C, zinc, magnesium and melatonin.
On the prevention side there’s also been very little in the way of consistent advice from health authorities on vitamin D as a preventative measure. Where the media or health authorities have made mention, the doses recommended are generally too low to make a difference. With the arrival of summer in northern climes, it’s a perfect time for people to get out in the sun to top up vitamin D levels. For those unable to take advantage of summer sun, vitamin D supplementation is a cheap and simple way to improve resilience and immune system function.
We share below a timely and important missive from our colleagues at the Orthomolecular Medicine News Service (OMNS) concerning evidence-based, very low cost recommendations for vitamin D supplementation. Maintaining optimal vitamin D status is especially important given the potential of a second Covid-19 wave later in the year.
- If we act on the data showing it is highly probable that vitamin D can save lives, we could fix this pandemic in a month, for perhaps $2 per person. There would be no significant adverse effects.
- If we wait for “evidence” that vitamin D mitigates the impact of Covid-19, thousands more will die
- If we did it and it failed, so what? The risk from not acting is much greater than the risk from acting
- Dosage is important and generally misunderstood.
Two countries have acted on this already, Egypt and Slovenia. Why can’t we?
The OMNS has been publicising the importance of vitamins D and C, and the minerals zinc and magnesium, in this pandemic since January [1]. I have been writing about Vitamin D and sunlight for over 30 years [2], and it has never been more relevant.
If you caught the Covid-19 virus right now, having a good vitamin D status (from taking a supplement already) would;
- Reduce your risk of the disease becoming severe by 90%
- Reduce your risk of dying by 96%.
This is not “proven” or “evidence-based” until we have done controlled trials comparing it to placebo. Any volunteers for that? But the data, already strong, has been pouring in since the start of the pandemic. Here’s the data for the two statements above.
[A Hazard Ratio of 4 means that in one condition, for instance vitamin D deficiency, you are 4 times more likely to suffer the “hazard” than in another condition, say vitamin D adequacy. The graphics are all mine.]
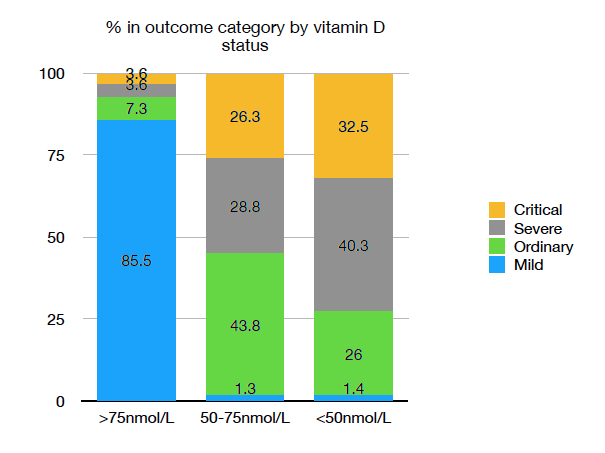
A Philippino study [3];
With a deficient vitamin D status (<50nmol/L) the probability of becoming Severe or Critical with Covid-19 was 72.8% against 7.2% with adequate vitamin D (>75nmol/L).
The Hazard Ratio is 10.0.
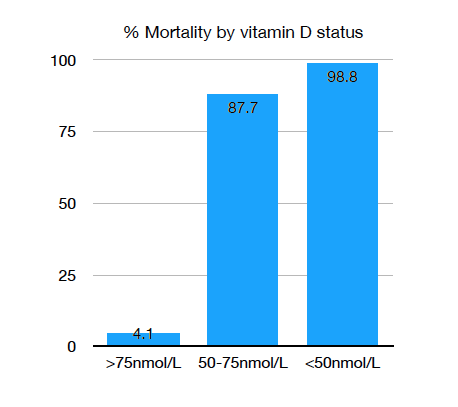
An Indonesian study [4];
With a deficient vitamin D status (<50nmol/L) the mortality rate from Covid-19 was 98.8% against 4.1% with adequate vitamin D (>75nmol/L).
The Hazard Ratio is 24.1.
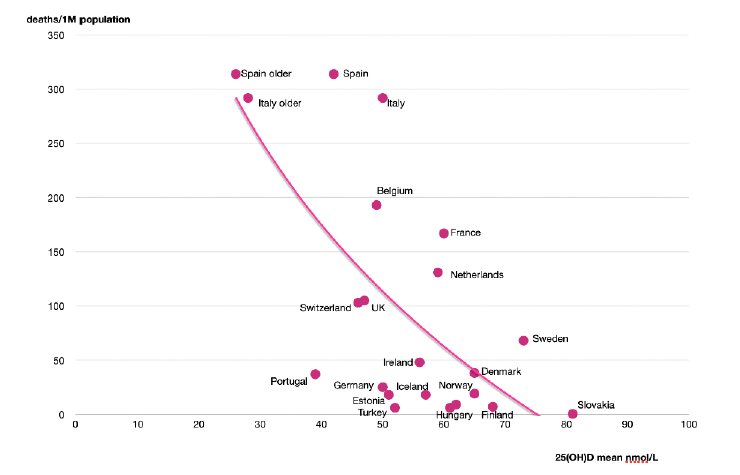
A review of data on Europe [5];
For countries in Europe the probability of developing Covid-19, and of dying from it, are negatively correlated with mean population vitamin D status, with both probabilities reaching zero above about 75nmol/L.
(The chart also shows the lower vitamin D levels for the elderly in Spain and Italy [6])
Dosage is important and generally misunderstood
Recent studies have suggested in discussion that more than 4000IU per day of vitamin D3 may carry a risk of harm, citing the UK Scientific Advisory Committee on Nutrition report of 2016 which set the recommended Upper Level (UL) intakes of 50mcg/2000iu per day. The report says; Excessive vitamin D intakes have, however, been shown to have toxic effects (Vieth, 2006).
However this is misleading, as the Vieth paper [7] states;
Published reports suggest toxicity may occur with 25(OH)D concentrations beyond 500 nmol/L
This leaves a wide margin of safety.
The 3 papers above show that a vitamin D3 blood level of 75 nmol/L is needed for protection against Covid-19. Government recommendations for vitamin D intake – 400IU/day for the UK and 600IU/day for the USA (800IU for >70 years) and the EU – are based primarily on bone health. This is woefully inadequate in the pandemic context. An adult will need to take 4000IU/day of vitamin D3 for 3 months to reliably achieve a 75 nmol/L level [9]. Persons of colour may need twice as much [8].
>>> Download PDF of OMNS article
References
- Saul Vitamin C Protects Against Coronavirus. OMNS January 26, 2020 http:// orthomolecular.org/resources/omns/v16n04.shtml
- Downing D. Day Light Arrow Books, London 1988
- Alipio MM. Vitamin D supplementation could possibly improve clinical outcomes of patients infected with Coronavirus-2019 (COVID- 2019). Preprint available at SSRN: https://ssrn.com/abstract=3571484
- Raharusuna P, Priambada S, Budiarti C et al. Patterns of COVID-19 Mortality and Vitamin D: An Indonesian Preprint available at SSRN: https:// papers.ssrn.com/sol3/papers.cfm?abstract_id=3585561#
- Ilie, , Stefanescu, S., Smith, L. The role of Vitamin D in the prevention of Coronavirus Disease 2019 infection and mortality. Square Research 2020. doi:10.21203/rs.3.rs-21211/v1.
- Lips P, Cashman K, Lamberg-Allardt C et al (2019) Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European Calcified Tissue Eur J Endocrinol 180:23–54
- Vieth R Critique of the considerations for establishing the tolerable upper intake level for vitamin D: critical need for revision upwards. J Nutr 2006; 136, 1117-1122.
- Vieth R, Chan PC, MacFarlane GD. Efficacy and safety of vitamin D(3) intake exceeding the lowest observed adverse effect level. Am J Clin Nutr 2001; 73: 288–
- Cashman KD, Ritz C, Adebayo FA, et al. Differences in the dietary requirement for vitamin D among Caucasian and East African women at Northern latitude. Eur J Nutr. 2019;58(6):2281-2291. doi:10.1007/s00394-018-1775-1






Comments
your voice counts
19 June 2020 at 1:58 pm
I have taken Vit D3 for nearly 30 years and have never had the flu. It works!
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences