Content Sections
Global status of reported Covid mortality
The World Health Organization (WHO), governments, the media and social media platforms have worked hand in hand to instil fear into citizens to maximise compliance with stringent and sometimes damaging strategies to counter the new coronavirus. Coordinating responses and messaging along with brutal censorship of those daring to disagree with the ‘party’ line.
Many will have become familiar with disappearing content on websites and social media streams. Below is an example of content removed from You Tube and in turn our website yesterday for “violating YouTube’s Terms and Services”. That’s what happens when censorship is controlled by private technology companies that now function as public utility services but choose to make their own, myopic, big business serving decisions to censor that they think constitutes harmful or misleading content. So much for freedom of expression and civil liberties in the so-called free world. It’s also why we’re rebuilding our own content on BitChute.
Familiar YouTube message on ANH-Intl website communicating the removal of a video of an interview with scientist and epidemiologist Knut Wittkowski PhD who questioned the need for lockdowns. Source: ANH International
-
Find related articles, information and videos in our Covid Zone
Ironically, the over-zealous censorship of free expression has now created the perfect conditions for such dissention to grow and develop. It’s almost become a game. Express dissenting views, have them removed and wait for people to reshare, then they’re removed again – and so goes the cycle.

One of many examples of censored podcasts – this one with Prof Dolores Cahill, Judy Mikovits PhD and Sherri Tenpenny
We’re told repeatedly governments are following ‘the science’ to justify lockdowns as being the only way to prevent hospitals being overburdened with catastrophic loss of life. But when you look at reported mortality rates (themselves varying country to country in how data are collected) you start to see a trend that doesn’t show pronounced benefits of lockdowns.
Below we’ve graphed the 25 countries with the highest rates of confirmed cases and then calculated the mortality rates per 100,000 population – which is a standard measure used for disease incidence. If you then look at a typical winter season in which combined deaths from pneumonia and influenza often hit in excess of 20 deaths per 100,000 inhabitants in a bad flu season, you’ll notice that only 9 countries in the world currently exceed this. That’s akin to saying the vast majority of countries have yet to experience mortality akin to a bad flu season.
But what you’ll also perhaps notice is that hard lockdowns don’t consistently produce low mortalities as might be expected – assuming you believe that lockdown is the most effective non-pharmaceutical intervention. In fact, there is no real relationship, with some countries that have had minimal lockdowns and no school closures having low mortality rates. The reasons why certain countries face much higher mortalities are likely highly complex and will include the age structure and health status of the population, the ability to shield vulnerable populations in care homes, the extent of natural immunity in the population, the timing of restrictions in relation to the arrival of the virus in a given country – and many other factors. What’s also becoming clearer is that most countries – irrespective of how they have reacted, are going through a classic 60 to 90 day cycle of elevated disease – the very pattern that most new epidemics of respiratory viruses undergo. It is simply the natural history of the disease.
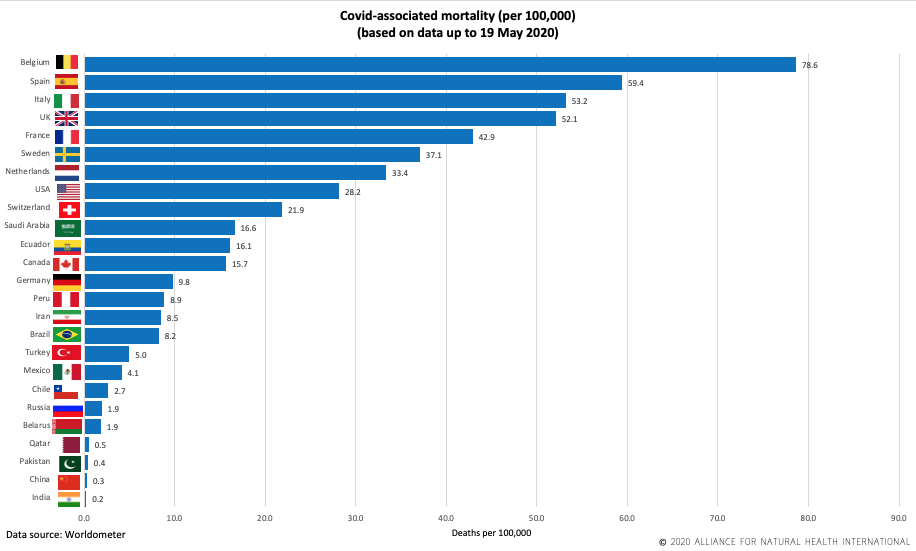
Covid associated mortality (per 100,000) (based on data up to 19 May 2020). Source: Worldometer
The 24/7 barrage of fear-inciting mainstream media coverage appears to have achieved its aim of making people terrified of the virus but we’re yet to count the toll on the economy and people’s health in general.
Testing, testing, testing
Even before it declared a pandemic the World Health Organization (WHO) was clear that testing strategies should be adopted “…to monitor transmission intensity” and that “Countries should prepare laboratory capacity to manage large-scale testing”. What’s happened in the real world has varied widely beween countries.
While countries report their testing progress to the WHO, they often do this in different ways. There are also many ways in which test numbers are artificially elevated. We’ve heard in the UK, for example, that it’s normal procedure when a single individual has had 3 tests to confirm presence of the disease using three different methods (e.g. salivary, pharyngeal and nasal), this is counted as 3 tests despite it delivering only one result – positive or negative.
-
We're funded only by donations. Any amount is welcomed to help us continue our work and make access free
The following figure shows the testing prevalence as a percentage of country populations in the 25 countries with the greatest number of reported tests. Here the relationship appears to be a little clearer – but not wholly consistent – with many countries that have tested higher numbers of their populations doing relatively better at minimising mortality. Belgium is an obvious outlier.

% of country population test (based on data up to 20 May 2020). Source: Worldometer
But what tests are we talking about, or, more accurately, are they talking about? Nearly all the publicly available data pertains only to antigen tests – the tests that tell you if currently have the disease, not antibody tests that tell you if you have had the disease and now likely carry immunity.
Confusion abounds both in the community but even among health professionals and policy makers over the type of test that should be used. There are also major questions over the reliability of the commonly used RT-PCR antigen tests. The roll-out of antibody tests, such as the new Roche antibody test or the Abbott antibody test look promising. Until you find the near-100% reliability that’s been cited by the manufacture has, as David Crowe revealed in an interview with health journalist and ANH friend Jerome Burne, a somewhat rickety undercarriage.
Another issue is who pays? Presently antibody tests are mainly available for limited research purposes or for those who can afford to pay privately. The efficacy of many are unknown with only a handful being awarded a CE Mark. Concerns are being expressed as to whether getting a positive result may make people less compliant with control measures.
To mask or not to mask, that is the question?
Current evidence suggests the main transmission route for Covid-19 is via respiratory droplets. However, there are conflicting opinions as to whether or not face masks provide suitable protection against coronavirus transmission. An increasing number of countries such as Venezuela, the Czech Republic, Austria, Turkey, Germany, Spain and France are now mandating the wearing of masks in various settings, with some also imposing fines for those caught not wearing one.
The evidence for masks as a means of protecting others is definitely inconsistent and sometime even contradictory. But as Zoe Harcombe PhD’s review of the evidence shows, there is an arguable balance of evidence tipped in favour of mask use in certain environments, particularly if there is a higher or unknown risk. In our view, this doesn’t apply around children and schools – this being the subject of our video piece also released today on why and how schools should reopen.
For many the wearing of a mask provides a way of dealing with an unknown ‘enemy’ and its associated hazards and risks. Something that provides a sense of confidence that allows them to feel in control, a symbol that shows they are protected while at the same time providing protection to others. Given the inconsistencies and somewhat weak scientific evidence, balanced against individual needs, concerns, vulnerabilities and exposure risks, we are in favour of choice for masks and other face coverings rather than compulsion. A recent modelling study suggests the benefits of wearing a face mask will be enhanced when used in conjunction with other non-pharmaceutical measures and use is universal (within nations). This kind of research will increase the likelihood of mask use being mandated in certain situations and given that masks make facial recognition more difficult, prepare to see this packaged alongside a drive for greater digital surveillance say via mobile phones.

An increasingly common pastime for furloughed workers.
There are also risks to the wearing of masks. Exhaled air can go into your eyes when wearing a mask, which can encourage you to touch your eyes potentially introducing the virus to your system. They can also make breathing more difficult, reducing the amount of oxygen available. Wearing a mask can induce anxiety in the wearer, which in turn can affect breathing patterns. When a mask becomes damp it increases the dampness in mucosal surfaces allowing greater opportunities for viral entry to the epidermis and subsequent viral replication. This in turn can increase the viral load a person is exposed to increasing their risk of becoming infected. It may also induce a false sense of security encouraging people to reduce hand-washing and other infection control measures.
The World Health Organization (WHO) advises “the use of a mask alone is insufficient to provide an adequate level of protection, and other measures should also be adopted”.
When using a mask it’s essential to use the correct techniques to put it on and take it off. Don’t touch a mask when wearing one and change single-use masks regularly or wash them frequently. The type and fit of a mask matters as well. One study found that whilst a surgical mask was 3 times more effective in blocking transmission than a homemade mask, using a homemade mask is better than no mask.
But, in recognition of the questionable evidence base, Dr Martin Marshall, Chair of the Royal College of General Practitioners (RCGP) in the UK said there’s no ”…evidence to support wearing a mask if you’re basically fit and well”.
Vitamin wake-up!
Our final update is on the mainstream media waking up to the importance of vitamins. That’s because the circumstantial evidence, as this Lancet Diabetes & Endocrinology piece suggests, has become overwhelming: those with very low vitamin D status have the most severe outcomes.
It’s also a reminder of the might and the messaging control exerted by the mainstream media and tech giants. Hundreds of quality posts on vitamins and their role in treatment or prevention, including our own, have suffered censorship at the hands of social media platforms when they were much more evidence-based than the lightweight recognition now being offered by mainstream media sources. But now the mainstream can express their views that vitamin D should probably be taken by everyone, low vitamin D status having found a place as a risk factor alongside obesity, type 2 diabetes and skin colour (the susceptibility of people from black and ethnic minority (BAME) backgrounds is of course in part related to vitamin D status).
Examples include articles in The Times , the Spectator and The Independent.
Some of the recent science includes:
- The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality
- The possible role of vitamin D in suppressing cytokine storm and associated mortality in COVID-19 patients
-
Rheumatologists' Perspective on Coronavirus Disease 19 (COVID-19) and Potential Therapeutic Targets
Even a SAGE advisor is now saying people need to expose themselves to sunlight to build vitamin D status – that’s after the public was previously advised to stay indoors. Ummm.
There are many issues here. How much body exposure, for how long, what effects might sunscreens or your skin colour have?
Sadly the government advice on vitamin D consumption flies in the face of the scientific evidence. The recommendation is for just 10 micrograms per day (400 international units). However, it is well known that individual requirements vary hugely - depending on such things as genetics (e.g. genetic variations affecting vitamin D receptors) and physiology. The only robust measure of status involves measuring circulating levels of the precursor, 25-hydroxyvitamin D, of the active form, 1,25 dihydroxy vitamin D, which is a hormone, the precursor to all our steroid pathways as well as being an anti-inflammatory agent and immune modulating factor.
Forty-eight of the world's leading vitamin D researchers agree that the optimal blood level for 25-hydroxyvitamin D is between 100 and 150 nmol/L (40 to 60 ng/ml). Vitamin D tests are widely available online and can be determined from a finger-prick/blood spot test.
To achieve these levels, for most adults this requires daily consumption of at least 10 ten times the recommendation given by governments - i.e. 100 micrograms (4000 IU) daily, in the absence of significant sun exposure.
Two historian's perspectives
We hear a lot of different perspectives on the Covid crisis from the scientific, political and economic community. Less so from historians. But surely a historical perspective is useful, given the long history over which humans have dealt with epidemics and infectious diseases?
We've selected two interesting interviews forrm leading historians. One being David Starkey, the other Prof Niall Ferguson (NOT the epidemiologist, note spelling of first name!).
Very interesting and relevant perspectives in our view.
Find out more at ANH-Intl's Covid Zone
Return to ANH-Intl homepage







Comments
your voice counts
22 May 2020 at 8:14 am
As always fantastic conclusive information ..feel anger more and more on our rights of freedom in terms of the lack of voices that the government doesnt listen to in its approach to the public and correct sources like yourselves. I was lucky enough to follow and understand covid and its implications on many aspects from yourself. The first time in the webinar series you did with other colleagues, and all family and friends follow the vitamins for immunity and we all listen and learn and feel properly educated in your continued resources. The school video this week is of particular use.i constantly share and often the information is taken down on social media sites ...but it doesnt stop me spreading the word...
22 May 2020 at 10:39 am
Thanks for the comment, Sarah. We're grateful you find our information useful - it makes us very frustrated that governments can keep on claiming they're being driven by the science - when this is patently not the case. Huge thanks for sharing our information as we cannot boost anything on social media given the restrictions imposed by platforms if view differ from those of governments.
22 May 2020 at 10:07 am
While I agree with your message I question the use of "When a mask becomes damp it can provide a humid habitat perfect for viral replication." This implies that there is viral replication within the mask whereas, like other viruses, replication only occurs within cells (because they make use of the cell's own machinery to do so). That said, warm and humid environments do favour bacterial replication so mask wearing might increase the risk of secondary infection..
22 May 2020 at 10:36 am
Absolutely right Jenny - it wasn't made clear enough. We've just updated the sentence to read: "When a mask becomes damp it increases the dampness of mucosal surfaces allowing greater opportunities for viral entry to the epidermis and subsequent viral replication." Thanks for spotting it!
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences