By Robert Verkerk PhD Executive and scientific director
Last Sunday saw the coming together of the UK Ayurvedic community in ways that were apparently unprecedented. Ayurveda has never quite found a comfortable foothold in the UK. There have been ideologies, approaches and personalities that have previously got in the way of a united front. Such tussles have perhaps compromised probably the longest surviving yet continuously evolving healthcare traditions.
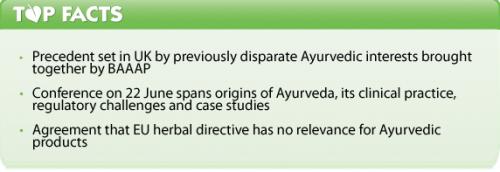
But when Dr Indira Anand, Chair of the British Association of Accredited Ayurvedic Practitioners (BAAAP) invited everyone she felt was significant to the UK effort on behalf of this great tradition, the response was overwhelming. This culminated in the Ayurveda Healthcare and Wellbeing Conference in Wembley, north-west London.

Dr Indira Anand, Chair, BAAAP
After Dr Anand’s opening, we, the audience, speakers included, were riveted by insights about the Ayurveda tradition and related Vedic wisdom by Sankrit scholar, Revd Dr Stephen Thompson. It's rare that someone of Caucasian origin can have this depth of understanding of an ancient language and Asian tradition, but it was no surprise to me that there are many Indians who have learned from Stephen Thompson. We were then taken on a whirlwind tour by various leading clinicians, including Dr Prasanna Kerur from the Ayush Wellness Spa in Jersey and Dr Ghanashyam Marda of the Maharashtra University, Pune, India. We then heard from a UK National Health Service consultant, specialising in the treatment of Alzheimer’s disease. His name was Dr Praddep Arya and he is a Member of the British Association of Physicians of Indian Origin. Interestingly Dr Arya made clear his thoughts that there was something wrong with the cover-up facing natural therapies and long-standing traditions. He tried to tackle the thorny issue of how Ayurveda might be better integrated into the mainstream healthcare in the UK. To support his case he cited various peer reviewed publications including one from the British Medical Journal in 2008 that showed that while there was no evidence cough medicine worked, there was some that suggested an Ayurvedic herbal mixture containing Andrographis did.
The elephant in the room
I felt Dr Anand was most insightful inviting three different speakers to discuss the regulatory challenges facing Ayurveda. Each had spent inordinate amounts of time on specific areas of the problem: Michael McIntyre on statutory regulation, Dr Dick Middleton on the EU traditional herbal medicinal products directive, and myself, trying to maintain the right to sell food supplements and prevent their removal from the market, by them being declared unnecessarily by EU or EU Member State authorities, as medicines or novel foods.
In an effort to cut to the chase, my main point to the gathered audience was that history has demonstrated that latching your wagon to any single approach is likely to be a risky strategy. Michael McIntyre would be the first to admit that, after 20 years of lobbying, consultations, enquiries and efforts to turn herbalism into a recognised profession, he’s still not sure how long it might take to yield his vision of a statutorily regulated profession. And the EU herbal directive, that was seen in the early 2000's as a means of securing the future of all manufactured herbal medicines, has failed dismally to provide a safe harbour for products of non-European traditions, such as Ayurveda or traditional Chinese medicine (TCM). Even the European Commission said the directive was inappropriate for traditional systems of medicine in its 2008 experience report.
So, here goes, the following are the key problems and our proposed solutions in summary form.
Primary barriers in UK/EU
- Products classified as unlicensed medicine (Directive 2001/83/EC, as amended) – definition and scope of definition of a medicine too broad and ECJ requires ‘case by case’ assessment by Member States
- Products classified as unauthorised novel foods (EU Regulation 258/97) – evidence of “significant use” prior to May 1997
- EU herbal directive (Dir 2004/24/EC) “not appropriate” – EC experience report 2008 (COM(2008).584.final)
- Inadequate guidance to Member States on safety of Ayurvedic herbs from European Food Safety Authority (EFSA) – Member States unclear of how to factor in public health concerns for individual herbs listed on EFSA ‘botanicals compendium’
- Unclear status of manufactured products used under ‘herbalists exemption’ (Regulation 3(6), 2012 Human Medicines Regulations)
- Non-medically qualified practitioners not considered “authorised health-care professionals” (Article 5, Directive 2001/93/EC)
Solutions proposed by ANH-Intl
- Achieve clearer delineation of food/medicine borderline for Ayurvedic herbs, minerals and other ingredients and finished products to create greater legal certainty over food supplements status
- Potential judicial review to secure precedents in European Court of Justice case law
- Coordinate safety evaluations of most important Ayurvedic herbs (ca. 80) presently missing from the EFSA compendium of botanicals in food supplements using a scientifically meaningful risk assessment approach
- Request that EC extends EFSA terms of reference to include evaluation of above risk assessments to deliver clear guidance for manufacturers and suppliers
- Support inclusion of herbs used in Ayurveda in the BELFRIT project and the EU-funded PlantLIBRA project
- Supply customs data of trade prior to May 1997 and help establish its use as evidence in novel food disputes
- Secure recognition by the UK’s Medicine and Healthcare products Regulatory Agency (MHRA) of Ayurvedic products suitable for use or prescription by different authorised health-care professionals in UK (Article 5, Directive 2001/83/EC as amended)
- Facilitate recognition by UK Herbal Medicines and Practitioners Working Group of diversity of Ayurvedic products suitable for use under exemption in Regulation 3(6) of 2012 Human Medicines Regulations
- Secure agreement from regulators for appropriate regulatory mechanisms for manufactured, complex products, often including mineral and other non-herbal ingredients, important to the tradition, such as food supplements and unlicensed ‘specials’
- Apply pressure on EC to establish new framework for traditional systems of medicine, including Ayurveda, as proposed in EC experience report (COM(2008).584.final)
Nationwide surveys of Ayurveda
While I feel it essential that we put this strategy onto the public record via our website, and cognisant of the maximum word limit we try to keep to for our stories, I do want to make one more mention of some crucially important information delivered at Sunday’s conference. It came from Ayurvedic practitioner and researcher, Dr Vijay Murthy who has divided his professional time between India, Australia, New Zealand and the UK. He spoke of the unique work carried out by the Australian Research Centre in Complementary and Integrative Medicine (ARCCIM).
He made a plea to the audience that all the Ayurvedic associations should bury their differences and come together as one and raise funds to conduct a national survey, in collaboration with ARCCIM. Why re-invent the wheel?

Dr Vijay Murthy, proposing a new way forward for clinical research integration
He made the crucial point that with a survey, subsequently published in a major peer-reviewed journal, there would be a solid latch on which to hook the Ayurveda wagon, something that has been sorely missed until now.
This is almost certainly an essential step for the recognition of Ayurveda as a valid system of healthcare, one that perhaps has more value today than ever before given the current epidemic of diet and lifestyle mediated diseases.








Comments
your voice counts
28 August 2014 at 8:15 am
It is indeed encouraging to note that world over the awareness about Ayurveda is increasing tremendously.It is due to the fact that Ayurveda is based on a very strong foothold of Philosophy and not a mere System of Medicine. It has withstood all the possible wars on it by the Pharma companies, hell bent upon making man a slave of medicinal products chemically produced and will further stand a witness to the human race.
At this juncture I feel that it is of utmost importance that we emphasize on educating the public and creating an awareness among them about their individuality and separate needs of medication. If there is a public demand for more of such tailor made medication the Government has to bow to their needs.
Secondly, we as Ayurveda practitioners must always remember that Research in Ayurveda cannot be based on the modern parameters of randomized study as the entire base of Ayurveda is individualized. In the last 22 years of my practice I have never come across 2 patients showing exactly similar patterns of disease though diagnosed under one disorder and have never been able to employ same medications in 2 similarly diagnosed cases. There are so many subtle differences that it is almost impossible to say that the cases are same.
Thirdly,herbs are very difficult to be standardized as their components vary in concentrations based on the geographical location, time and season of collection.
The subtleness and vastness of Ayurveda cannot be measured by the modern technology since the design is Divine.Congratulations to those associated and best wishes for all the members. We really need to work together globally.
03 September 2014 at 6:25 pm
We definitely need to work together for this awareness indeed Dr. Neelesh. This healthy alternative to medicine is at the forefront of the battle against addictive "cures" to conditions and diseases. This in-depth article the 4000 year old Ayurveda tradition, made by Dr. Jacqueline Miodownik-Aisenberg, is inspiring and enlightening; give it a look please: http://www.vidamd.com/vida-intel/ancient-roots-how-to-relieve-stress-naturally-with-ayurveda/
10 October 2015 at 10:54 am
Hello, Sir,
I stumble across your website on Google and found it very informative and engaging. I would like to tell you that I also like to share my ideas with people around and feel your website is the perfect place to deliver them. So it’s my humble request to you to kindly grant me the permission so that I can also post some really creative and fresh content written by our experts of Ayurvedic doctors.
You can see my previous articles here.
https://www.curejoy.com/expert/Drvikram
www.drvikram.com
Subscribe our blog & youtube channel For the latest new updates & Real Testimonial by the Patients who Treated Successfully in Ayurveda
Youtube Channel : https://goo.gl/2JKCsK
Do reply
Regards
Planet Ayurveda
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences