After this brief video introduction, you’ll find the first part of the script Rob Verkerk prepared for the first part of his presentation at the Thought Leaders Consortium of the Personalized Lifestyle Medicine Institute.
This year’s theme introduced by PLMI President, Jeff Bland PhD, was ‘Personalizing Nutrition Therapy in the Age of Lifestyle Medicine’.
In summing up at the end of the packed two-day schedule, Dr Bland referred to this seventh annual PLMI conference as the “best one yet”.
It's a pleasure to have the opportunity to speak to you all this morning at this year’s conference. Very briefly, I come at this issue as a biologist, ecologist and sustainability scientist. That's what I've been doing for the last 35 plus years of my career, both in academia and the non-profit sector.
So let's ask this question: what is healthcare?
For most it's the delivery of products and services intended to manage disease or deal with trauma. It occurs largely in specific human-made structures we call clinics and hospitals. But it also reflects particular types of business models, politics, economics, globalisation - and of course attitudes, expectations – and, very importantly yet so often ignored, belief systems.
Speaking of belief systems - because humans have become so technologically focused since the Industrial Revolution, many still pin their hopes on magic technological bullets. The hope – for many – is that new drugs and treatments will soon emerge to resolve the escalating rates of chronic, degenerative, and autoimmune diseases. Then there’s also the need to contend with the rising tide of infectious diseases that are resistant to current antibiotics.
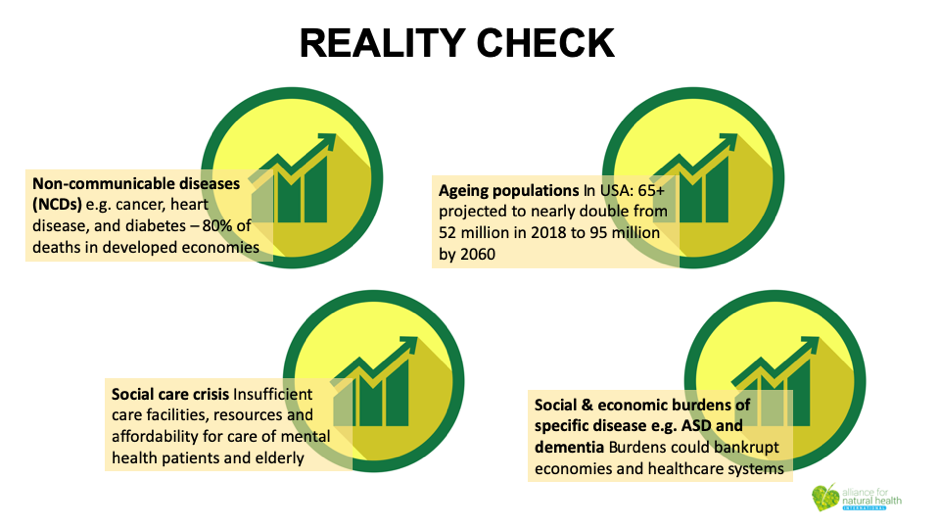 Whichever way we look at it, the current model of 'healthcare’ is failing us. When you look at predictions of the future, it becomes really disconcerting. Drug pipelines in key areas, such as antibiotics, are almost empty. There are, for instance, just 800 scientists in the global pharma industry currently working on antibiotics that might be capable of dealing with the current AMR [antimicrobial resistance] crisis.
Whichever way we look at it, the current model of 'healthcare’ is failing us. When you look at predictions of the future, it becomes really disconcerting. Drug pipelines in key areas, such as antibiotics, are almost empty. There are, for instance, just 800 scientists in the global pharma industry currently working on antibiotics that might be capable of dealing with the current AMR [antimicrobial resistance] crisis.
One thing that's becoming clear the world over is that these diseases all have complex upstream causes, and are a function of gene-environment interactions and a complex interplay of physiological, social and environmental determinants of health.
So if we’re to prevent disease, or better still, regenerate health as opposed to just managing diseases and symptoms – this being an entirely unsustainable option given the predicted global burden – we have to alter our mindsets dramatically. We can no longer rely on the prospect of highly targeted, new-to-nature molecules – even biologics, or vaccines, two of the biggest growth areas for pharma – coming to the rescue.
‘Precision medicine’ became all the rage after the launch of Obama's Precision Medicine Initiative in 2015. It started with big ideas, it was synonymous with personalized medicine, combining genomics with big data analytics and population health. Today it's already been derailed by pharma. Most doctors, as a result, see it simply as a system that allows better targeting of drugs to specific individuals. The lifestyle and nutrition angle, the two biggest determinants of health itself, are often side lined.
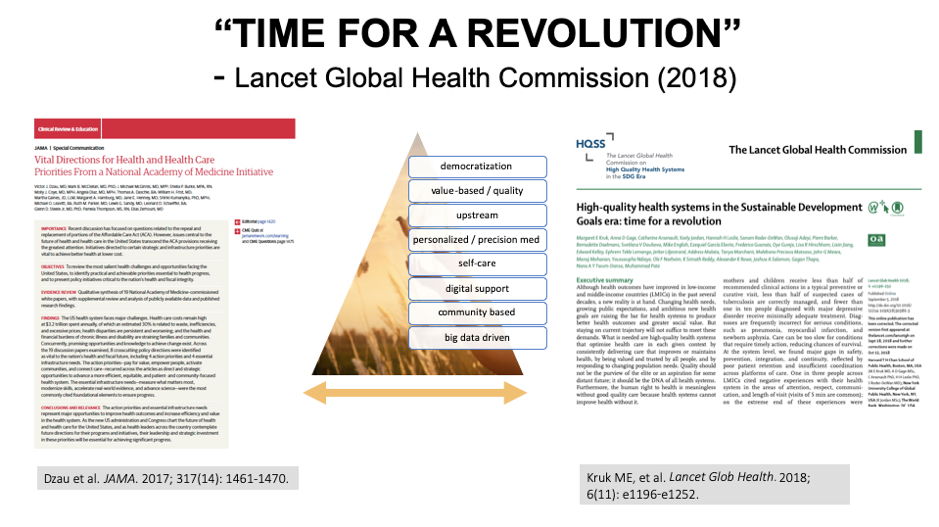
Coming out of that was the Vital Directions initiative from the National Academy of Medicine, headed by Victor Dzau, Mark McClellan and others. The series of discussion papers acknowledges that massive reform in how we do healthcare is needed urgently. It acknowledges that you need to activate communities and empower people – that most health care actually happens in the community, not in clinics and hospitals.
We've also seen the publication of the findings of a Lancet Commission on Global Health last year. It recognises the Sustainable Development Goals of the UN, SDG 3 being focused not on disease but on 'good health and well-being’. But when you read the smallprint, you can see pharma has already had its way. Pharma’s take on disease prevention is vaccination – so it sees this SDG as a huge opportunity. That’s why it lobbied the World Health Organization to make vaccine hesitancy one of the top 10 global health threats.
Both these big picture views have a number of things in common, things that are essential to any sustainable reform of health ecosystems. That includes the democratization of health, value-based and quality, upstream, personalized, precision medicine, self-care, more digitization, and community-based, big data driven health systems.
As pharma-based business models are the prevailing business models, we must also recognise the influence of accountants and management consultants of the ilk of Deloitte and McKinsey that help steer these in the delivery of healthcare products and services.
The latest report by Deloitte recognises the instability of health economies. Being accountants, their focus is on creating financial stability for the sector.
It begs the question, who is this for; businesses or citizens? For the betterment of healthcare quality among the majority of us – citizens – should we be looking for financial stability, or should we be looking to create more sustainable health systems that function robustly even in uncertain economies? Perhaps a thought given the political instability we face under the rule of people like Donald Trump and Boris Johnson.
So let's go on to look briefly at some of the overwhelming trends linked to personalized healthcare about which there is very wide consensus.
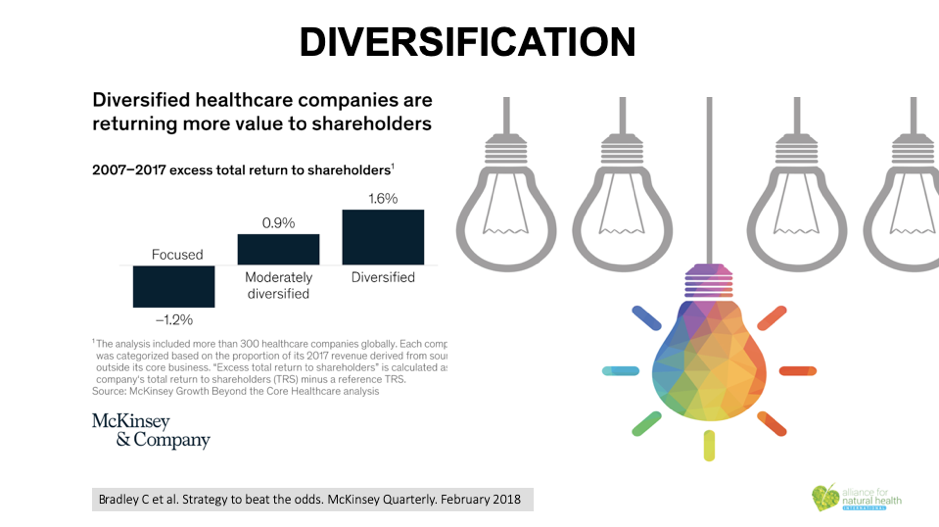
Here – from McKinsey – we see a real plug for diversification of existing business models. Remember when the tobacco industry was forced to diversify? That was because the main business model – selling cigarettes and tobacco – was beginning to fail. The fossil fuel energy companies are in the same situation today. It happens when the prevailing business model is no longer delivering the same value to shareholders.
You might be familiar with the Three Horizons model pioneered by the International Futures Forum. It shows that when the first horizon is gone, and you're digging deep into new innovations to develop the second horizon, you're still some way off a much more sustainable third horizon.
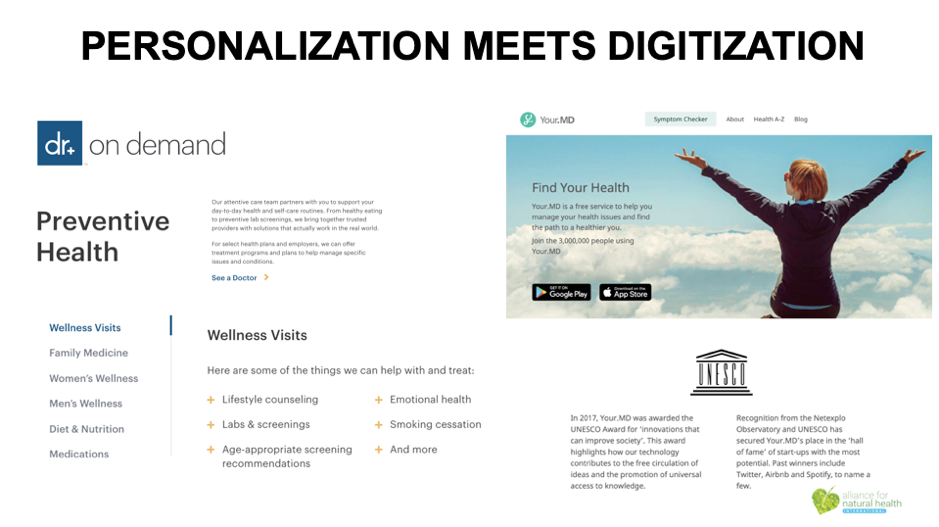
Another trend that’s unstoppable is the digitization of health. Yes, it's necessarily technologically driven, but it can also be very empowering and motivating. When we have numbers that describe aspects of our health, we can track our progress better. We can orientate better from a state of worse health, or system function, to better health or function.
But let's also not ignore some of the potential downsides. Three come straight to mind. The first is a big one that relates to data ownership. When your data disappears to a cloud, do you know who owns it or who has access to your data? Do you really want an insurance company or a government to know your every heartbeat or blood glucose or insulin response? Think about what the consequences could be. We strongly support systems that rely on citizen-owned, not company-owned, data.
Another issue relates to the unprioritized and somewhat random emergence of specific technologies or monitoring systems. When a company or app builder succeeds in releasing something that works, it's not necessarily because it's monitoring the most important function. It's often because it was simply technically feasible to do that and build a business model around it.
Thirdly, there’s the affect that digital connection has on us and the albeit ironic potential for us to disconnect from real people, rather than connect further. Digitisation in primary care is already disconnecting doctors from their patients, doing damage to the value of the therapeutic relationship in the process. Many doctors today spend more time staring at their screens than they do building relationships with their patients so they can really serve their needs.
Check out Business Insider Intelligence’s Digital Health Ecosystems report and you’ll see just who’s coming to the party. Whether it’s providers or payers, governments or device makers, there’s massive growth in this sector – all capitalising on your and my health data. We need to be careful with whom we share our data. The bottom line is this – if you don’t know, don’t share.
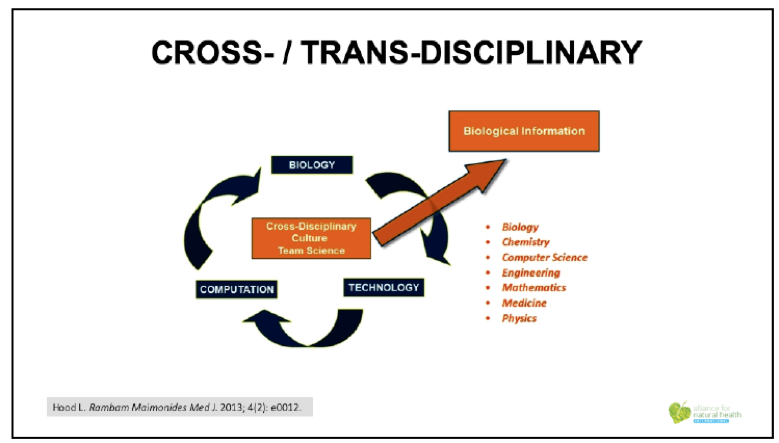
Another trend is that health systems are becoming not only cross-disciplinary, but also trans-disciplinary. This is a good thing, and hopefully starts the process of moving Western medicine out of the siloes it’s been in for close to a century.
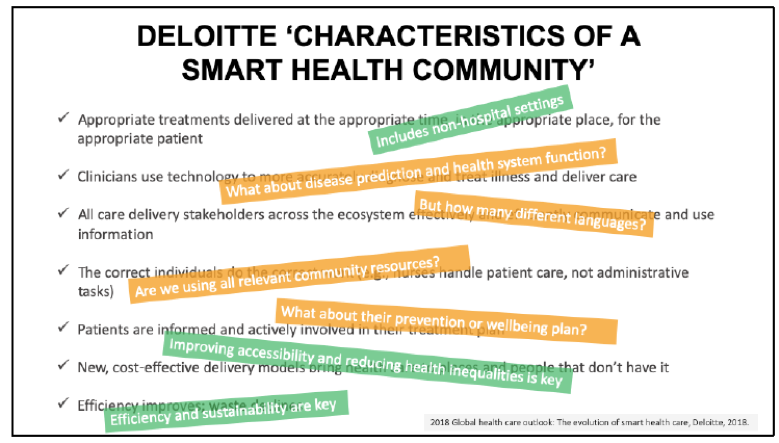
Deloitte is also well aware that so-called smart health communities are going to be part of our future. But again, its assumptions aren’t necessarily ones that will encompass diverse, sustainable health systems in which there is respect for people and our relationship with nature. Deloitte’s view of a smart health community still doesn’t see citizens as empowered individuals, working with the support of their communities to increase healthspan and optimise health. Proactive health care that’s about health creation using nutrition, lifestyle and other non-pharmaceutical approaches, is of course the most sustainable kind of healthcare. But it’s not that popular with pharma and pharma interests as it means that most people can avoid using medications for most of their lives.
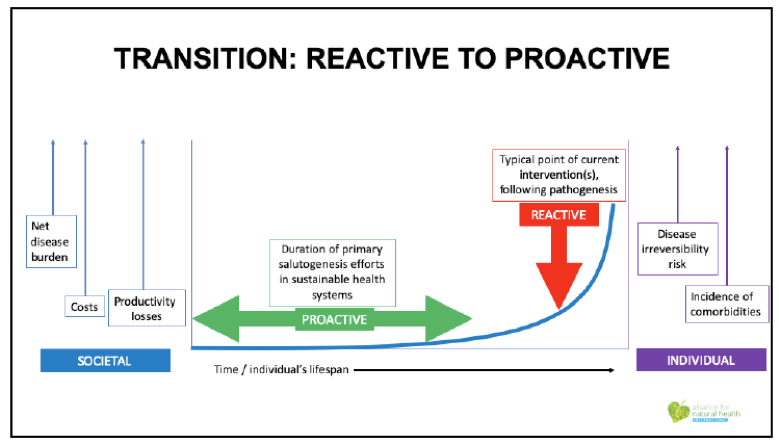
This is why we need to transition from a reactive approach to healthcare to a proactive one. The present business model means you don’t do a lot until disease has been diagnosed. Then you receive interventions, often later in life when you’ve often got more than one disease, delivered by people who are trained largely to deliver drugs and surgery. These medical doctors – presently – don’t in the main have the background or band width to do much to help people get their health into balance.
It’s a little like saying let’s only go to the smash repair outfit to service our car, even though the smash repairer deals largely in panel beating and spray painting, and doesn’t know too much about the subtleties of engine management systems. We rely on the wrong people for the job, that mostly needs to happen in communities, outside the physical structures associated with mainstream medicine, the hospitals and clinics.
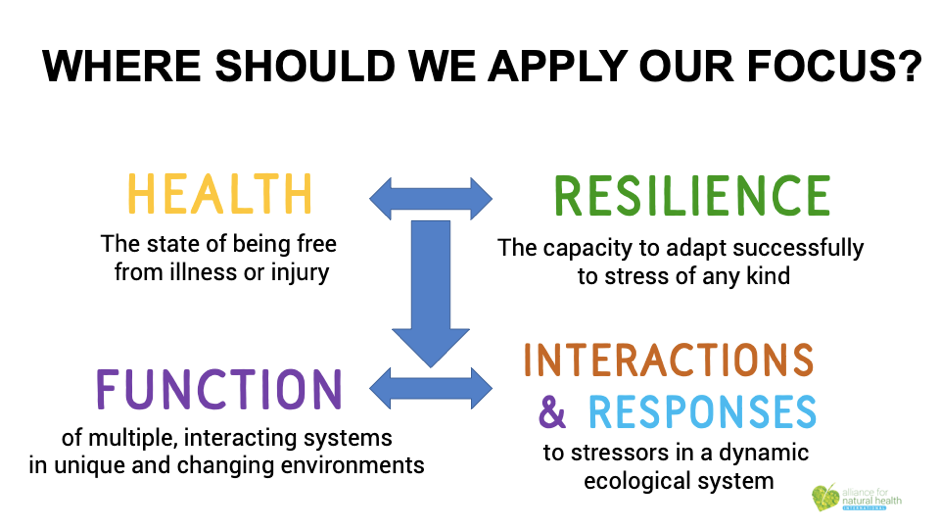 We need to focus much more on resilience than just being free from illness or injury. We also need to focus more on the specific function of different body systems and the interactions and responses we experience to stressors and other elements in the dynamic ecological systems in which we’re a part.
We need to focus much more on resilience than just being free from illness or injury. We also need to focus more on the specific function of different body systems and the interactions and responses we experience to stressors and other elements in the dynamic ecological systems in which we’re a part.
Naming diseases and then trying to tame them with drugs or surgery isn’t really healthcare. It’s disease management – and that’s what we’ve been doing on a large scale for the last half century or so and it’s no longer working for us.

This takes us back to the kind of metrics we need to describe our state of health and resilience. Yes, at some level, it’s useful to quantify some of who we are. But let's not forget some of the much more subjective drivers of health and resilience. Take our psychosocial and emotional health, for example. Or what get’s you out of bed in the morning; what the Japanese refer to as ‘Ikigai’. These are softer markers that are not less important. They can be a lot more important than parameters like cholesterol levels that are often managed closely, not because they’re the best way of preventing heart disease, but rather because they help support the prescription of drugs such as statins.
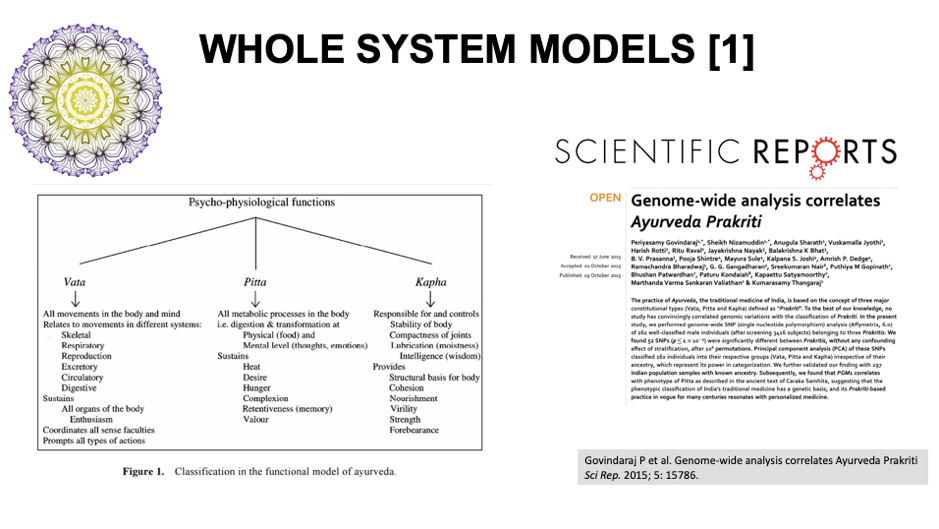
This takes us to whole system models of health. The oldest we know of is the great 4000 plus year-old, Indian tradition of Ayurveda. It’s amazing that the ‘prakriti’ which includes the three doshas, namely vata, pitta and kapha, have now been substantiated by modern genetic evidence.
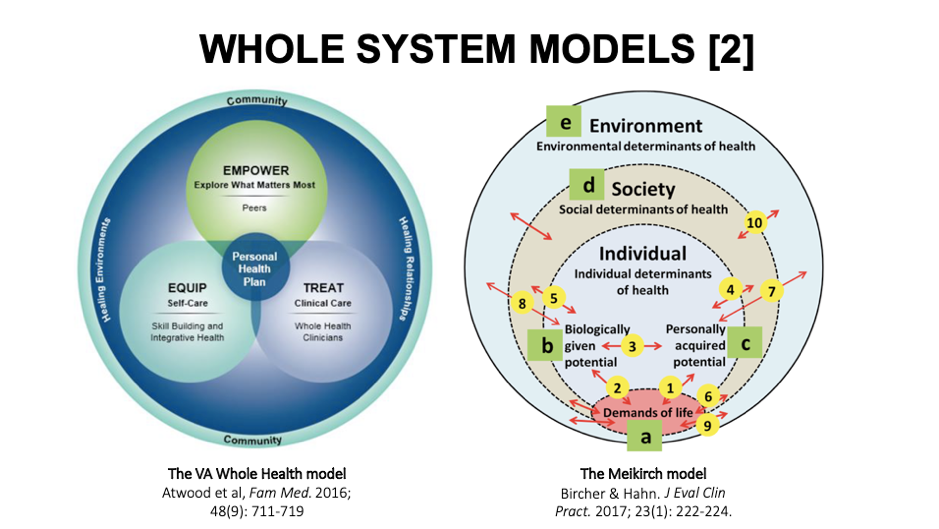
Then you’ve got the Whole Health model now used on the biggest healthcare system in the US, that of the Veterans Administration (VA). It’s personalised and centres on empowerment, self-care and treatment that focuses on the whole person. Although under attack by skeptics, Reiki, acupuncture and other natural therapies are offered as part of veterans’ medical benefits package.
The Meikirch model was born in a Swiss village by a group of doctors looking for better ways of helping their patients understand their bodies as adaptive systems with multiple points at which specific behaviours and interventions can influence health. All of the pressure points and interactions are distilled into 5 domains and 10 interactions, all of them actionable.
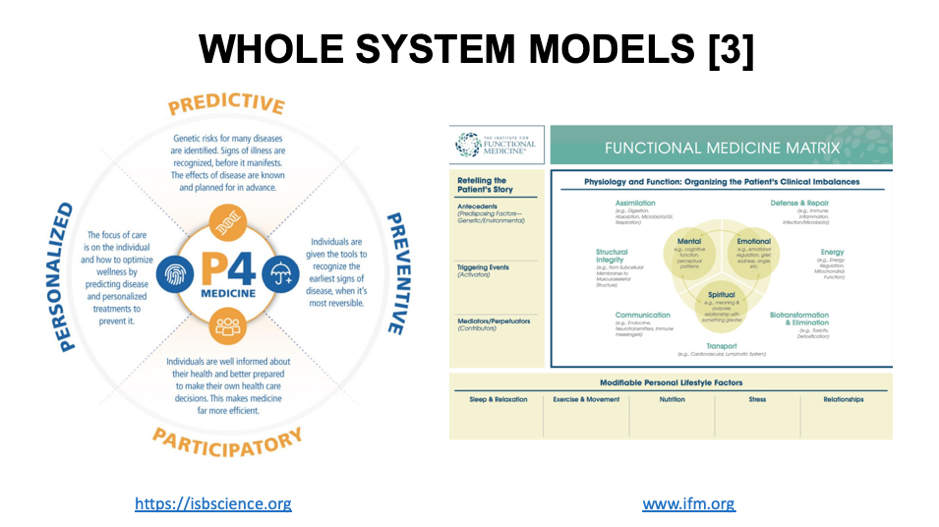
The final two whole health models that we should mention, that have been discussed already at this conference and are well known to everyone here, is Dr Lee Hood’s P4 Medicine model and the Functional Medicine model developed through the Institute for Functional Medicine, and co-founded by Dr Jeff Bland.
The former is more about providing a context for the development of strategies and technologies that are amenable to a systems biology approach to medicine. The latter is more about a model that has proven itself over the last two decades as being very helpful when used by practitioners to guide patients and clients through the key systems that can be manipulated to manifest improved function and better health outcomes in cases of complex, chronic diseases.
Rob spent the second half of his presentation talking about the ANH blueprint for health system sustainability, about which you’ll find more information on our website.







Comments
your voice counts
There are currently no comments on this post.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences