In a break away from the past conference convention, health charity, the College of Medicine held its 2016 conference on food and medicine. Acknowledging the impacts of diet and lifestyle choices on health, this was a first for conventional clinicians in the UK. It was a conference orchestrated by clinicians for healthcare professionals with a desire to understand how food can be used to prevent and treat different problems and diseases. The conference aimed to provide clinicians with the necessary resources and information to bring a new dimension to their delivery of medicine. It was a dynamic conference focused on bringing about effective change at every level. Robert Verkerk PhD and Meleni Aldridge from ANH-Intl attended alongside some of the most inspiring doctors driving change in UK mainstream healthcare.

From left to right: Dr Rupy Aujla, Dr Rob Verkerk, Meleni Aldridge, Dr Rangan Chatterjee
Driving health change
Many of us who have long embraced natural healthcare have an innate trust in the human body’s ability to find health. We look at our food and environment as resources that we can alter to give our bodies the best chance of doing what it’s designed to do – to achieve an optimal state of health and resilience. We tend not to opt for new-to-nature pharmaceuticals, or visit the doctor, as the first option when we’re feeling off colour. So it was a landmark moment being amongst mainstream health professionals at such a marker-in-the-sand conference. For some it was their first exposure to the concept of food as medicine and MC, doctor and comedian, Phil Hammond, couldn’t have been a better choice to guide the day. The selected line up of expert speakers hit their mark time and again ensuring the day was replete with light bulb moments for those new to the subject matter.
Master of Ceremonies, Dr Phil Hammond
Those of us with a strong belief in the power of natural health are a growing force in the market place, as well as socially and politically. We tend to frequent health stores, with many of us ignoring most of the aisles in the supermarkets offering products we’d rather not put in or on our bodies. We often also look in horror at the kids’ menus in restaurants. Who was it who decided it was OK to give kids inferior foods to those on the adult menu?
When our choices are questioned by the majority, who still think mainstream medicine and pharmaceuticals offer the best tools for managing our health, we sometimes feel like we’ve got an uphill battle if we're to do the 'right thing' and offer evidence-based justifications.
The reality is that evidence-based medicine has been distorted from its originally intended meaning. Most doctors and health authorities take it to mean results from double-blind, randomised controlled trials (RCTs). The patient’s experience is almost entirely ignored.
As it happens, much of the evidence for even mainstream drug or surgical treatments is conflicting or weak. Belief systems and experiences tend to be more important influences. The scientific journal and evidence-based medicine resource, Clinical Evidence, has so far evaluated the efficacy of 3000 medical treatments in common use and found that only 11% have been proven to be beneficial with a surprising 50% of unknown effectiveness. The time couldn’t be more ripe to see our mainstream healthcare systems getting with the food and lifestyle medicine programme. This conference was well timed, well aimed, and most reassuringly, welcomed.
Diet and lifestyle at the pinnacle of change
If you’ve never tried natural health (because drugs have always been your go-to option), why would you change your mind especially after reading newspaper headlines claiming vitamin supplements don’t work, or worse, vitamins might actually increase your risk of death! Those of us ‘in the know’ understand that headlines like this are spun from trials that don’t reflect how most of us use supplements. We understand also that the vitamin supplements that have been used in some of the negative trials are very high dose synthetic forms that aren’t necessarily like the ones we might choose to use. We also know there is a gamut of other trials with positive findings out there that don’t get blasted across the media. And probably most importantly, we have experienced the benefits of making carefully considered choices in terms of what we eat and how we prepare our foods, when and how much we eat and what kinds and amounts of supplements we take.
The average mainstream general practitioner is still largely lukewarm over food supplements. Often misinterpreting a number of studies on isolated, synthetic vitamins and applying these to all kinds of supplements including botanicals, amino acids and food-form, body-ready, vitamins and minerals.
Most, however, through the sheer weight of science in its favour, are coming around to the notion that dietary and lifestyle choices are among the most important determinants affecting any person’s long-term health. They increasingly recognise that our risk of developing chronic diseases such as type 2 diabetes, obesity and even dementia are strongly linked to long-term trends in what and how we eat, and how we behave. This was repeatedly borne out in last week’s conference, which was a sell-out months before the event with a long waiting list.
 1
1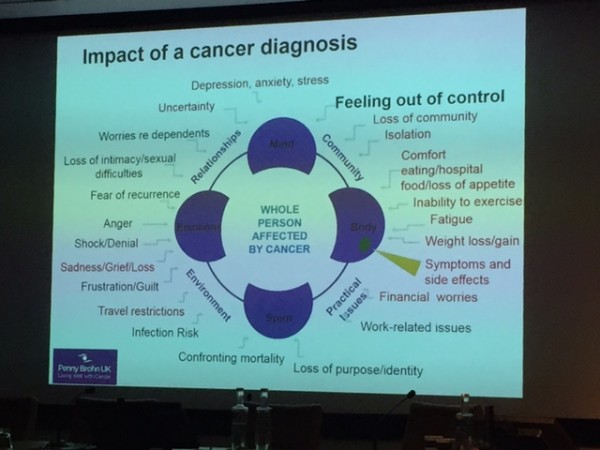 2
2
Dr Catherine Zollman presents a whole life approach to cancer
The challenge is that far too many clinicians still don’t know what diet and lifestyle approaches to prescribe or recommend to individual patients – and they spend too much effort tackling health problems too late in the disease cycle. But with none of these issues featuring in the medical curriculum, should we be surprised that most doctors have little knowledge or experience in this rapidly emerging area of nutritional and lifestyle medicine?
Collaborating for change
Last week’s conference confirmed that we’re beginning to see some shifts in how the mainstream medicine community handles this dilemma. One such shift is the increasing openness to using non-medically qualified health professionals, such as nutritional practitioners, health coaches and personal trainers, in general practice clinics. Progressive primary care physicians or general practitioners (GPs) wishing to impart life-changing information, in the typically NHS-allotted 10-minute time frame per patient, have an insurmountable task if they are solely responsible.
These GPs are disrupting the classic doctor-patient stereotype. As we shared last week, new models are being built on a foundation of teamwork and empowerment shared between the doctor, his or her collaborating team of health professionals — and, centrally, the patient. During this process, unlike the current conventional model, the patient takes leadership and ownership of his or her own health. One such movement that is helping to drive these shifts is the Functional Forum, led by US-based, British entrepreneur, James Maskell.
Peer-led patient focus groups are also being organised by practice managers so that patients with common disorders can come together and spend longer periods of time with suitably qualified and experienced health professionals who can guide and coach them, as well as inspire patients to help each other. Patients who are seeing a doctor or practitioner who acknowledges that food is medicine and good lifestyle choices are the foundation of health are in good hands. Those who are not, might ask if their healthcare professional might be interested in subscribing to “the world’s largest integrative medicine conference” or joining organisations such as the College of Medicine or the Institute for Functional Medicine. It’s a genuine and powerful movement for positive change who’s time has definitely come.
When healthcare delivers positive, empowering and life-changing results experienced by the patient, who needs RCTs? At the very end of the conference, this was very well summed up in powerful words by Crohn's patient and patient representative, Carrie Grant (well known in the UK as a TV presenter, vocal coach and session singer). Carrie made an impassioned call for clinicians to cultivate a flexible mind set, to become good coaches and to form collaborations using diverse teams of health professionals to deliver all relevant information to the patient so the patient can be fully engaged and take full responsibility. But she also underlined the need to be gracious in the leadership position and then teach others to be good leaders. Patients no longer want the ‘doctor as God’ model, they want to be empowered to create change in their own lives and take responsibility for their health through working in partnership with their healthcare professionals.
While speakers struggled to find agreement on how much fat was needed in a health diet, if nothing else, the College of Medicine conference signposts exciting times ahead!
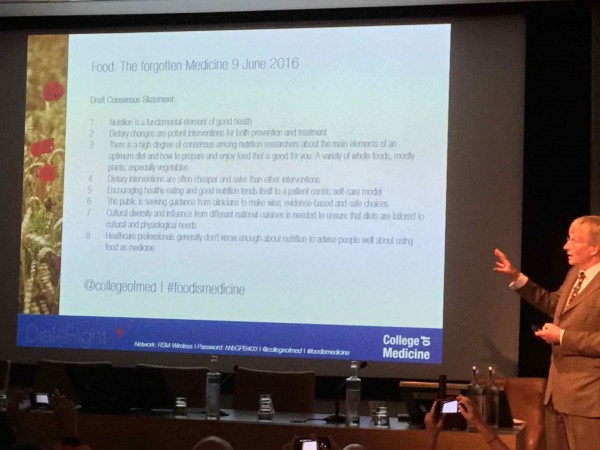
Dr Phil Hammond presents the draft consensus statement at the end of the conference
Draft Consensus Statement:
1. Nutrition is a fundamental element of good health.
2. Dietary changes are potent interventions for both prevention and treatment.
3. There is a high degree of consensus among nutrition researchers about the main elements of an optimum diet and how to prepare and enjoy food that is good for you: A variety of whole foods, mostly plants, especially vegetables.
4. Dietary interventions are often cheaper safer than other interventions.
5. Encouraging healthy eating and good nutrition lends itself to a patient centric self-care model.
6. The public is seeking guidance from clinicians to make wise, evidence-based and safe choices.
7. Cultural diversity and influence from different national cuisines is needed to ensure that diets are tailored to cultural and physiological needs.
8. Healthcare professionals generally don’t know enough about nutrition to advise people well about using food as medicine.







Comments
your voice counts
16 June 2016 at 10:11 am
Good news - any chance of the consensus statement being written up?
23 June 2016 at 12:42 pm
Hi Michael,
We have added a typed verison of the consensus statement to the end of the story and also emailed you.
Many thanks,
Susie
17 June 2016 at 3:43 pm
Check out an amazing new site that makes using food as medicine completely accessible - www.checkyourfood.com
17 June 2016 at 10:40 pm
so excited to see these changes coming to fruition. Can we spread the word to places like Africa where the middle classes are getting fatter because fast food is becoming the norm there...?
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences