Content Sections
By Meleni Aldridge, executive coordinator, ANH-Intl
I wouldn’t call myself a blogger. In fact, I’ve never written a blog before. So forgive me if I transgress any blogging boundaries in ignorance. My motivation for taking up the blogging baton today is driven by two reasons. Firstly, having not drawn on the NHS for over a decade, I’ve had a couple of unexpected and unforeseen health challenges this year. For someone who’s really into self-care and knows a fair bit about how to keep my health on the right track, it’s been hugely frustrating to not be able to DI(m)Y it this time.
I’ve known for well over a decade that the NHS is buckling and failing to cope - hence my propensity for DI(m)Y health in the first place. And I work for ANH for goodness sake. We work in this space, researching and educating on how to better manage health by working with nature, not against it. We’ve even developed a new model that’s about changing the way we should access health care that’s all about building functional, sustainable health systems. It’s all about re-imagining what health and care should be all about, taking the pressure off the mainstream system – so when you really need it (because you’ve just been run over by a bus), it’s there for you.

Meleni Aldridge BSc(Nutr Med) DipCPNI CertLTFHE.
Wake up, smell the coffee…
For me, it’s taken this first-hand experience to really bring home to me just how desperate the ‘healthcare’ situation actually is. The NHS isn’t just buckling, it’s already mortally wounded. And it needs us to make rapid changes if we want to keep it from collapsing altogether. In this country [the UK], the might and the majesty of the NHS is part of the culture. It’s woven firmly into our DNA and it seems we do all – me included – have an expectation that it will be there for us when we need it most. I wish I could say it had been.
I know my experiences aren’t isolated, nor are they the most extreme or serious. People talk and I’m hearing a similar theme all too often now. The difference being that many of those people don’t have the benefit of knowing how to self-care or the money or knowledge to seek other expert options. So, my second reason for writing today is to look at how different my experience would have been if the ANH’s model of a sustainable health system was already in place.
My experience of medical failure
Whilst I can’t fault the speed of response for my first health challenge earlier this year when it was thought that it might be something serious and life-altering (which it wasn’t thankfully), the same can’t be said when the problem is deemed non-life-threatening. Yet, non-life-threatening conditions can also be acute and they can really impact things that are important to society and the economy like someone’s ability to work productively.
Having spent so much of my adult life as a practitioner focused on health creation, to me, anything acute needs immediate attention. Partly because of the pain and discomfort, but also to prevent further damage and provide the best chance for a full recovery. In my case, I’ve managed to herniate one and possibly two lumbar discs, causing a level of nerve compression that has taken me to a dimension of stratospheric pain I didn’t know existed. Plus, not unnaturally bringing a complete halt to my probably (ok, definitely…) over-busy life. The timing and the deeper somatic ‘message’ that my body is sending me has not been lost, just in case you were wondering if I was deaf to the deeper red flag.
I was unlucky that my problem became acute over a weekend when my GP practice was closed. Not overly given to drama or wanting to deplete NHS resources further, I avoided A&E and hung on till Monday to see my doctor. Having not been a drain on the system and never needed to access expensive diagnostics before, I was hoping for an MRI to find out what was causing such extreme pain. Frankly, I was also looking for some heavy-duty pharmaceutical relief. The latter being incredibly rare for me, but very necessary at the time.
Instead, I found out that GPs can no longer refer patients for MRIs and my ‘urgent’ appointment for an assessment at the nearest hospital’s musculoskeletal clinic is 8 weeks away. This is just for the initial outpatient appointment, not the MRI. In the meantime, my GP practice has informed me that they won’t be issuing any more prescriptions for the pain meds as they (opioids) are potentially addictive.
Good call, more action is definitely needed to prevent opioid addiction. But could it be that some of the addiction occurs because people are forced to stay on these potent pain-relieving meds simply because they’re having to wait months for even the first step in treatment to occur? In my case, I didn’t get a physical examination by the doctor on my first visit, just an eyeball once-over that confirmed that I was indeed needing a prescription for meds. I couldn’t sit down, was standing at an odd angle and could barely breathe for the pain. In the current UK system, there’s nothing else that can be done until the assessment at the musculoskeletal clinic 2 months away, yet my pain prescription was initially for 4 days, which was helpfully extended for another 4 days. That’s still 7 out of 8 weeks that I’m expected to manage on my own, with no advice, support or prescription meds.
Health the sustainable way
In the individualised, tailor-made, health system that we’ve outlined in our blueprint, we, the citizens (the word patient makes me feel helpless and disempowered) access our health and its care in a different way. Wider access with more choice of health professionals than just your GP being your only port of call other than A&E or a walk-in centre. More than that, we can choose among a diverse range of health and fitness professionals that all share the same common language. Whilst I acknowledge this is going to take time, political will, extra effort and education, it will put each of us so much more in the driving seat of our own health and take enormous pressure off overworked and overstressed GPs.
You might not be aware that in the UK, other registered health professionals outnumber doctors by more than 2 to 1 and that figure is increasing as more GPs leave the profession due to burnout.
In my health example, I needed to be seen immediately by a musculoskeletal expert and then get a script from the GP. The 4 to 8 days of drug therapy would be wholly appropriate because the right kind of physical assessment and treatment early on means that you resolve quicker.
There are many different kinds of musculoskeletal experts out there, but there’s usually only physiotherapy on offer through the NHS. I have derived huge benefit on this occasion from some very hands-on therapy from an osteopath. His expanded toolbox of clinical skills have been perfect for my current condition. But I’ve had to fork out privately despite being up-to-date with my taxes that should really have been able to give me the patient-centred care described in the NHS Constitution for England. That’s not to say that on another occasion a physio, rehab practitioner or a masseur might not be what I need. And that’s only talking physical, musculoskeletal issues. Imagine having the same kind of choices across all 12 domains of your personal ecological system?
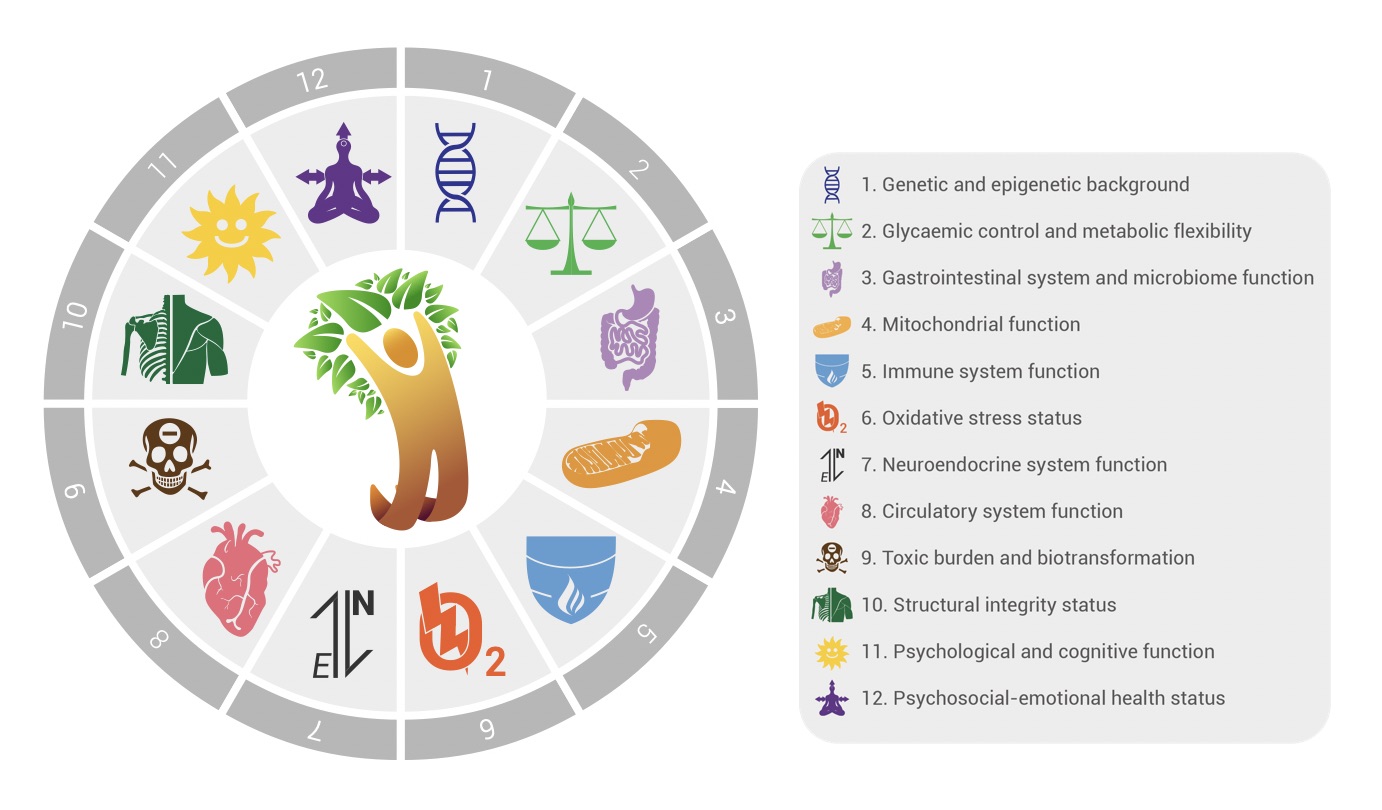
The 12 domains 'Ecological Terrain' from ANH-Intl's Blueprint for Health System Sustainability.
Let’s get into the driving seat of our own health
Thankfully, instead of facing months of agony waiting to be assessed for the next step in my treatment, my quick access to the very experienced osteopath I saw has meant positive change in a matter of days. His decades of clinical experience – and the huge difference he’s made to my pain and mobility – has given me confidence that his suspicion over what’s driving and triggering my problem is likely spot on. I’d still like an MRI and so would he, so I’ll wait for my clinic appointment. But in 2 months I’ll probably be so much better that an MRI might be off the table. Or it will be waste of taxpayer’s money, mine included.
We need this new model of health care and not just because we (ANH), are its creators, but because we passionately believe it’s the model best equipped to make healthcare systems future-fit. We also desperately need to get away from the ‘pill for an ill’ model that is still so dominant. We need to change our focus from the treatment of symptoms of disease – disease management – to the creation of health. This means altering our behaviour, our diets, our lifestyles, how we relate to each other, and to the environment around us. All of the science and clinical experience tell us that prescription and over-the-counter meds simply aren’t up there among the top priorities when it comes to long-term health creation.
We also need to take the pressure off mainstream healthcare delivery systems like the NHS so they can be allowed to do what they do best. That’s especially around the treatment of acute disease and injury.
All of us need a functioning health service that’s there for us when we need it, because we never know when that time will be. It’s time for a proper, no holds barred, reality (health) check because the NHS and mainstream healthcare delivery systems like it, just can’t continue without radical change.
Find out more about our blueprint for health system sustainability.







Comments
your voice counts
18 July 2019 at 4:09 pm
While one can frame this in terms of the NHS - the underlying issue is the regulatory capture of health science by pharmaceuticals.
Captured revenue streams under corporate and government laws, becomes a population 'pharmed' for sickness.
The underside of this is that the 'many' are deeply afraid of pain of loss and are willing to sacrifice '(health) freedom for power of protection. Many such 'answers' propagate the problem they are supposed to fix - perhaps into more complex or subtle forms of displacement. The 'protectors' can then become dealers to a current incapacity or unwillingness to address and own our life experience so as to prioritise sustainability for a persistent wilful or unconscious misalignment.
Self-awakening - as a re-educative willingness - and self-responsibility AS a relational wholeness - is fundamental.
Regenerative embodiment of health and wholeness in active expression are the context of such an awakening shift.
The intent and attempt to GET RID of the hated self is the generation of a split mind under narrative control of conflict management. I know this is 'deeper' than the current social narrative is open to consider - but after many months of disabling back and sciatic pain I accessed an 'out-of-time' insight of trying to get rid of something ETERNAL. This is another way of saying I was opened (or got out of the way) to a recognition of a self-futility - beneath or 'inside' my usual sense of self, life and time.
In our social context - pharma has been at the fore of the attempt to eradicate, block or deny symptoms assigned to generic diseases - where every instance is a unique expression of a relational context.
In terms of reaping as we sow - the attempt to eradicate, block or deny living feedback (or true messengers), is fuelling a top-down canopy of denial - in which the dissonance GROWS - and thus attracts greater demand or dictate of CONTROL.
There may be a recognition - not in surface thinking - but in the heart's knowing - that we are (one with) the problem - until we are one with the release or resolving of the problem. Surface thinking is fitted and for the protection and survival of a self-separateness, set over and against the heart's knowing or wholeness of being as an alloy of love and hate.
'Too big to fail', is indicative of false investments seeking sustainability by outsourcing the cost onto 'others' and 'world'.
Perhaps the only way to re-open a recognition and remembering of the true - is to withdraw allegiance and protection or support from the false, and if this is so, then we will generate 'crisis' towards finding and living our willingness - and breaking the 'spell'.
Crisis brings both danger of fear-reactive entanglement AND opportunity for yielding and embodying wholeness - depending on our active purpose. Under fear and threat of loss of 'healthcare', manipulative re-distributions of psychic-emotional energy operate ever diminishing returns as a systemic denial of true relational being and all that shares or partakes of it.
Yielding to truth is not really something we can set out to 'do' - but invested illusion can be brought to notice by its dissonance.
But studying or setting up crusades against the symptoms of dissonance will not actually heal but truly realigning will - regardless the persistence of symptoms. I am talking of the mind that is besieged by its own convictions.
If we are to find ourself progressively denied, then are we being driven to unlock resources we may not yet believe or be able to imagine? Manufactured systemic sustainability is not our Sustenance - but a substitute for life as a system of 'control' masking over fear and its progeny. Alignment in health is in relational resonance to the Call to Live - and not the call to war in fears flagged to a dissonance.
The Greek pharmakoi, singular pharmakos, refers to victims who were ritually beaten, driven out of cities, and killed, for example, by being forced over the edge of a precipice. The word pharmakos, designating a person who is selected as a ritual victim, is related to pharmakon, which means both "remedy" and "poison," depending on the context. In the story of the horrible miracle of Apollonius, the beggar is a pharmakos, a kind of ritual victim. Apollonius points to him as the demon causing the plague (he is the source of pollution or poison), but his lynching restores the well being of Ephesus (he becomes the remedy for the crisis).” — Trans. René Girard,
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences