Content Sections
It’s a common view that the ‘complete lockdown’ many of us are still enduring was our only option. There’s very little focus on what might have been - or even on what might still be, in terms of how we exit from lockdown. What the natural course of the disease would have been without full lockdown? Especially if we’d elected to pump way more resources into testing as well as focusing on shielding vulnerable older populations – leaving the rest of society to get on with life.
Tomas Peuyo’s article that espouses a ‘hammer and dance’ strategy has had 40 million views, has been translated into 30 different languages, and forms the basis of a petition to the White House. Pueyo’s ‘hammer’ is the non-pharmaceutical lockdown measures we’ve recently become so familiar with, while the ‘dance’ refers to the longer-term strategies for managing the disease, notably vaccines.
-
Find related articles, information and videos in our Covid Zone
There’s little talk of another hammer – which might include better ways of managing severe disease among the small proportion affected in this way, while simultaneously preventing critical care facilities from being overrun. This would likely still include selective deployment of non-pharmaceutical measures such as social distancing and shielding of vulnerable populations.
If you could substantially reduce the number of deaths among that very small proportion of those infected with SARS-CoV-2 who become seriously ill in critical care units in hospitals, we could all go back to life as usual once this first wave of the pandemic has passed. The evidence (below) points to the fact that most of the world is already over the hump (see Figure below).
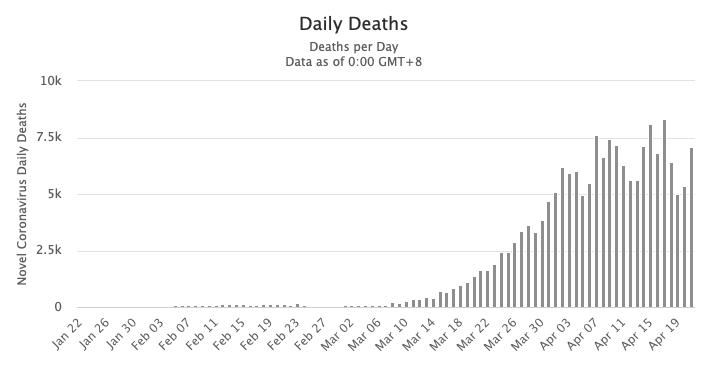 Daily death rate from Covid-19 (as of 22 April 2020). Source: Worldometer
Daily death rate from Covid-19 (as of 22 April 2020). Source: Worldometer
It’s a big ask of course – and there’s no doubt that critical care doctors are doing their best within the bounds of their resources, knowledge base, experience and permitted codes of practice. It’s also the first time for many that they’re dealing with a novel disease that can be particularly ravaging among the elderly and those with underlying diseases.
But are citizens infected with Covid-19 and suffering severe disease getting the best possible care and treatments?
Variation in outcomes
What is emerging is that there are considerable variations both between different countries and between different combinations of strategies in critical care facilities. It’s not within our remit here to discuss all of the options available, but it is of great importance that there is wild variation between survival rates in different countries and critical care units. This can be down to many factors, including different strains (there are currently at least 3), different population susceptibilities and different exposure levels, to mention just three variables.
UK intensive care units don’t currently seem to be the safest places to be sent with serious Covid-19 illness. The UK’s Intensive Care National Audit and Research Centre (ICNARC) continues to report that only about half those entering critical care come out alive (see ICNARC report, 17 April 2020). Three quarters have a BMI of 25 or more and around the same proportion are male. There is no push from the UK government to help people, especially men, to lose weight or reduce their risk of hypertension or metabolic diseases – that could reduce their susceptibility dramatically. By comparison, in a study of patients admitted to critical care units in Hong Kong, only 22% died.
What’s more – the majority of the literature emerging on novel therapeutics involves re-purposing existing therapeutic agents (e.g. hydroxychloroquine, chloroquine, corticosteroids) or looking at novel therapeutic agents (remdesivir, favipiravir, lopinavir) or vaccines. This bias appears to be driven more by the business model that can exploit the Covid-19 phenomenon than the genuine needs and welfare of citizens.
Patented synthetic versus unpatented natural
Herein lies one of the most fundamental challenges: the rivalry between patented therapeutic approaches and use of unpatented natural agents that have demonstrated high levels of success in the hands of those clinicians who have used them to help save lives.
With a novel viral disease with a capacity to kill significant numbers, positive results derived from the ‘art’ of medicine as well as clinical experience, knowledge and expertise are hugely significant.
Embracing approaches borne out of such knowledge and experience casts into the wind the evidence-based medicine model that most doctors have been taught to uphold throughout their careers: that you need highly powered, multi-centre randomised clinical trials, and ideally meta-analyses of these, before you can determine the best therapeutic strategy.
Outside the box
But when doctors are faced with doing the best for their patients, especially if not constrained by the system in which they work as is the case with privately-funded, integrative medicine doctors, a different process can take precedence.
For these doctors, there’s generally a deep understanding of a known or likely mechanism for why an agent might work which triggers its use in the first place. There’s usually also experience with similar diseases with related modes of action. Then, when a doctor or group of doctors are able to demonstrate outcomes that appear to stop patients with severe disease from dying, the word gets out (unless it’s interfered with through censorship). Like most doctors, they are enthusiastic fans of the Hippocratic Oath, and they believe there’s just not enough time to wait for randomised clinical trials to be conducted before they deploy what they consider to be safe and medically plausible therapies.
Looking at the mainstream end of critical care, this very approach has led to a recognition that mechanical ventilators may not be the saviour they were first thought to be in critical care. This is because Covid-19 patients respond very differently to those with non-Covid viral pneumonia and the majority of mechanically ventilated Covid-19 patients tend to die (88% in a JAMA published study of hospitalised patients in the New York City Area).
Conversely – there are interesting data showing the importance of other agents and approaches that don’t involve patented medicines that are at risk of being demoted in value – simply because they are not patented and therefore not supported by commercial interests. That is the way the biomedical model has worked for the last 60 or so years and this needs to be recognised at a time when people – sometimes including our loved ones – might be dying unnecessarily.
In another article published today, we take a closer look at some of the natural treatments marginalised by mainstream medical interests that brave, forward-thinking doctors are using to help save lives.
Find out more on ANH-Intl's Covid Zone







Comments
your voice counts
There are currently no comments on this post.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences