Content Sections
By Robert Verkerk PhD, Founder, executive & scientific director
While researchers around the world have been exploring the many risk factors linked to the risk of severe disease or death from covid-19, governments by and large have limited most of their attention to very few. Their primary emphasis has been on a ‘hide-then-vaccinate’ strategy that aims to try to reduce transmission of SARS-CoV-2 until such time one or more safe and effective vaccines have been developed.
This strategy is in itself risky and emerging evidence is that lockdown might not be as effective as some claim. The effectiveness and the safety of Covid vaccines is currently unknown, and there is no certainty of either.
From whales, penguins and polar bears – to health
When faced with uncertainty and risk, a common sense strategy involves carrying out a thorough evaluation of all options, looking at risks and benefits, then choosing what appear to be the most appropriate options that minimise risk to people or planet. Where there is a high level of uncertainty, the precautionary principle, that has long been invoked to help protect endangered species and habitats, can be applied. That’s what the World Health Organization’s interpretation of the precautionary principle, as applied to human health, has dictated since 2004.
It states: “…in the case of serious or irreversible threats to the health of humans or the ecosystem, acknowledged scientific uncertainty should not be used as a reason to postpone preventive measures.”
Do preventive measures only involve trying to reduce transmission and developing vaccines? Have the risks and benefits of these been properly assessed in relation to other potential strategies? The answer is 'no', and huge uncertainty remains around each of these approaches.
Our recognition of the myopic strategy being taken by governments triggered our attempt to identify some of the other factors that are known scientifically to affect risk of severe disease or death from Covid-19 disease, 52 of which are listed below. We regard asymptomatic, mild or even moderate symptoms of the disease as irrelevant to any justification of a global pandemic strategy, such as that controlled and coordinated by the Geneva-based World Health Organization and World Economic Forum.
Token risk assessment
As Ortwin Renn indicates in his chapter on the precautionary principle in the Reference Module in Earth Systems and Environmental Sciences (2015), a precautionary approach or a risk-based approach are typically taken when uncertainty prevails around major issues affecting environmental, consumer and health protection. In the UK, it seems neither approach has been used. While a traditional risk assessment approach has been put forward by the Health and Safety Executive (HSE), it has been oriented specifically towards companies rather than individuals or the health professions. It also fails to address many of the modifiable risk factors other than transmission - or exposure-related risks. It also leaves the assessment up to individual companies.
The Big 52
At ANH-Intl, we’ve identified 52 factors that have been linked to risk for severe disease or death from covid-19, these being divided into 7 groups (Fig. 1). Of these 7 groups of factors that affect disease, health, metabolism, nutrition, social or working conditions, and the natural environment around an individual, on average 54% of risk factors in each group are considered modifiable. A further 36% are considered possibly modifiable, leaving just 11% as generally not modifiable (see Table below).
Factors include age, gender and underlying conditions, in addition to well-recognised social or environmental determinants of health, such as social deprivation and air pollution. But they also include less well recognised metabolic, nutritional and behavioural factors that can have profound impacts on the risk of serious covid-19 disease.

Figure 1. Fifty two factors that influence an individual’s risk to severe covid-19 disease and death, categorised according to the typical ease by which each factor is modifiable.
Table. Summary of risks of severe covid-19 disease and death showing the percentage of three categories of risk that relate to 7 groups of factors
|
|
RISK FACTORS FOR SEVERE COVID DISEASE & DEATH |
||
|
Modifiable |
Possibly modifiable |
Generally not modifiable |
|
|
Health factors (n = 12) |
42 |
17 |
42 |
|
Disease factors (n = 12) |
42 |
42 |
17 |
|
Metabolic factors (n = 7) |
86 |
14 |
0 |
|
Nutritional factors (n = 7) |
100 |
0 |
0 |
|
Social factors (n = 6) |
33 |
50 |
17 |
|
Occupational factors (n = 5) |
40 |
60 |
0 |
|
Environmental factors (n = 3) |
33 |
67 |
0 |
|
Average percentage |
54% |
36% |
11% |
*Sum of percentages may not equal 100 owing to rounding.
Skating on thin legal ice
Ignoring these factors given the status of knowledge about their effect on risk could be considered tantamount to negligence by governments and may represent a breach of the duty of care by governments under tort law. Medical doctors who have not provided the appropriate standard of care to covid-19 patients, because, for example, they were highly vulnerable by virtue of their age and were not transferred to intensive care (critical care) units, a fact revealed by The Sunday Times last weekend, may also be found to be clinically negligent.
Reasons for government neglect
Of all the factors, it is the nutritional and metabolic factors that are by far the most modifiable (see Figure 1 and Table). So why so little attention by governments?
There are many reasons for government failure to prioritise the many things that could greatly affect people’s risk of serious disease or death, failures that will definitely be costing lives, including:
- Governments have consistently failed to recognise the big picture, trans-disciplinary nature of the multiple factors that influence risk of serious covid-19 disease, preferring to focus on trying to break the transmission cycle and developing a vaccine
- Siloed experts. Medical and scientific experts advising governments are generally weighted towards epidemiologists, modellers, statisticians or behavioural scientists with a limited grasp of nutritional and environmental factors that affect immune resistance, tolerance or resilience
- Mis-delegation. Mainstream medicine has long ago delegated the responsibility for nutrition and related health sciences to dietitians whose practice has been slow to integrate developments in the nutritional sciences. Hence this profession’s failure to impact the rapid increase in incidence of metabolic diseases like type 2 diabetes and obesity that are in turn a major reason for the vulnerability of significant sectors of the population to covid-19 disease
- Locus of control. Focusing on modifiable risk factors places the locus of control back on individuals and communities and away from governments. That’s something governments don’t want as they try to assert control over populations to enact, through the Great Reset, the greatest societal transition since the Industrial Revolution of the late 1800s
- Time and inequity. Modifying the risk by an individual may take time and people’s capacity to modify risks will vary according to their knowledge base, support and education, as well as their social, cultural and economic conditions or circumstances.
Only the final point is a possible justification for accepting the need for, or ignoring the collateral damage associated with lockdowns and social distancing. It is certainly not sufficient reason to not engage in trialling broader strategies that aim to build immunity in the population.
Putting all your eggs in just two baskets
If you focus global efforts on only one disease, in this case Covid-19, and you conclude that the disease has a high degree of lethality and you fail to recognise there are therapeutic solutions to the disease, you can potentially justify shutting down societies and decimating economies to save lives. Unfortunately, neither of these assumptions are right. Regarding lethality, there was a period of time when some countries, the UK, some European countries, the USA and South American countries, suffered higher than average mortality that was likely linked to infection by SARS-CoV-2. But this is presently historic, as highlighted by EuroMOMO data and latest ‘Nightingale’ plot by the Centre for Evidence-Based Medicine at Oxford University.
While ‘cases’, as determined by positive PCR tests, in many parts of the world are again rising, it is still too early to predict with any degree of accuracy how many of these will be found to translate to covid-19 disease, hospitalisations and deaths. Getting a clear view of this will in any event always be clouded by symptoms being shared with other respiratory diseases and the murky classification of covid-related deaths.
The other flawed assumption is that there is no effective treatment. Dr Paul Marik and other emergency doctors in the US have developed a sound scientific and medical rationale for what’s called the MATH+ protocol (Fig. 2) that includes corticosteroids, anticoagulants, antivirals and immune supporting nutrients, including vitamin C, thiamin (vitamin B1), zinc, vitamin D, magnesium and melatonin. Clinical evidence has suggested mortality rates among critically ill patients treated using this protocol is considerably less than 10%, a mortality rate that’s significantly lower than standard care approaches.
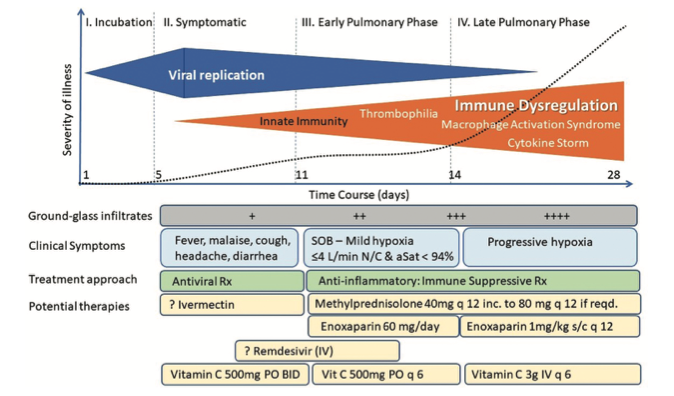
Figure 2. Typical course and stages of Covid-19 disease with associated treatment plan according to the MATH+ protocol. Source: Marik et al.Expert Review of Anti-infective Therapy, DOI:10.1080/14787210.2020.1808462.
Governments shouldn’t of course just be doing risk assessments that focus on covid-19. They need to consider the implications of all measures and policies they implement on all facets of society. And it’s this fundamental difference in outlook between, on the one hand, the ‘covid myopic’ governmental approach, and, on the other hand, the big picture view of public health, as espoused by the scientists behind the Great Barrington Declaration, that leads to such polarised views of what should be done.
What’s more, why look only at risk? What about benefit? At ANH, we’ve long been pushing for a transition away from risk assessment towards risk/benefit assessment wherever circumstances being assessed are likely to involve both risks and benefits for health. It’s an approach that doesn’t just apply to things like vitamins that are both good for us in some forms and doses, but can be harmful in certain forms and doses too. It should be just as applicable for dealing with the current global crisis around covid-19.
Risk/benefit assessment would mean the collateral damage caused by lockdown and related measures designed to protect populations from covid-19 would have to be factored in. This is the very issue that the Great Barrington Declaration scientists, now supported by over 11,000 medical and public health scientists, 32,000 doctors and nearly 600,000 concerned citizens, have been calling for. As Dr Scott Atlas, a public health scientist advising The White House said in an interview with Unherd.com, “We must open up because we’re killing people.”
Dr Atlas crystallised some of the statistics that graphically highlight the secondary impacts of lockdowns as follows:
“In the US, 46% of the six most common cancers were not diagnosed during the shutdown… These are people who will present to the hospital or their doctor with later stage disease — many of these people will die. 650,000 Americans are on chemotherapy — half of them didn’t come in for their chemo because they were afraid. Two-thirds of screenings for cancer were not done; half of childhood immunisations did not get done; 85% of living organ transplants did not get done. And then we see the other harms: 200,000 cases plus of child abuse in the US during the two months of spring school closures were not reported because schools are the number one agency where abuse is noticed; we have one out of four American young adults, college age, who thought of killing themselves in the month of June…”
Collateral benefits
There is a potentially more sinister reason why governments are averse to risk/benefit assessment of the possible options that go beyond the ‘hide-then-vaccinate’ strategy that has become the mainstay of nearly all governments. Not only would they have to face head-on the extent of the damage that is being wreaked on societies the world over in their efforts to break the cycle of transmission up until such time a safe and effective vaccine is ready. They’d also have to consider the collateral benefits of any multi-stranded approach that prioritised modifiable risk factors. That includes the very strategies they have so long resisted or failed at: improving nutritional status and metabolic function.
Then there’s the real sting in the tail: if you help populations to improve their nutritional status and metabolic function in order to reduce susceptibility to Covid-19, you simultaneously reduce the risk of almost every single chronic and autoimmune disease. These include heart disease, cancer, obesity, type 2 diabetes, dementia and a rash of autoimmune disease like Crohn’s, rheumatoid arthritis and ulcerative colitis, that have, prior to the emergence of covid-19, been seen as diseases that might break modern healthcare systems. That might be exactly what governments don’t want, given the size and might of the pharmaceutical industry, that depends on an ageing, chronically diseased populations.
That also might explain why governments prefer collateral damage to collateral benefits.
Let’s start at the very beginning
There is no way any government will take on all, or possibly any, of the responsibility to help support their populations in modifying their risk in the face of the current and topical infectious disease threat. But there’s no harm in trying to force their hand, if for no other reason to ensure they don’t ignore the wider science, politics and economics that would allow for a more just and democratic society.
We make this point on the day we launch our vitamin D campaign, in which we ask the UK Health Minister to consider donating vitamin D supplements to those in deprived communities who are likely to be most deficient in the vitamin, and least able to to justify supplementation. The measure would involve a tiny investment compared with the millions involved in running test and trace programmes, or providing support for communities devastated by job losses and other effects of draconian policies.
Taking back control
But our key advice is this: please don’t wait for your government to decide. We might just need to wait a lifetime or more. Wherever we can, let’s make the decisions that seem most relevant to us. Doing things that involve minimal cost that deliver significant benefits – such as adults taking 5000 international units (IU) (125 micrograms per day) daily, or better still, getting yourself tested and then supplementing to get your circulating levels of 25-hydroxyvitamin D into the optimal zone for immune support. Find out more in our Vitamin D campaign.
We urge you to look carefully at the array of factors we’ve detailed in Figure 1. Self-care is where so much healthcare is going – and so much of this is in your control. In the health space, you might need the guidance of a health profession. But the travesty is you generally won’t find the right guidance from a conventionally-trained medical doctor or physician. You will however find it from a wide range of non-conventionally trained health professionals, such as functional medicine practitioners, herbalists, practitioners of traditional systems of medicine (Ayurveda, traditional Chinese medicine), and many other disciplines. It is for this very reason we see it as so critical to progress turning our blueprint for health system sustainability into reality.
We are currently engaged in organising a major conference in London for 2021 on this theme – we’ll keep you posted as arrangements progress.
>>> Visit covidzone.org
>>> Navigate to our new 'Test & Take: Vitamin D' campaign
>>> Return to ANH homepage
>>>> Subscribe to our newsletter







Comments
your voice counts
18 November 2020 at 7:27 pm
A very interesting article which emphasises the importance of taking responsibility for one's own health. In particulate avoiding addictions such as drugs, alcohol and smoking. Taking positive action such as activity (also exercise), and healthy eating to avoid obesity.
In Britain the successful anti-smoking campaign should become a healthy lifestyle campaign. The avoidance of risk and achievement of benefit to our health is in some part in our own control.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences