Content Sections
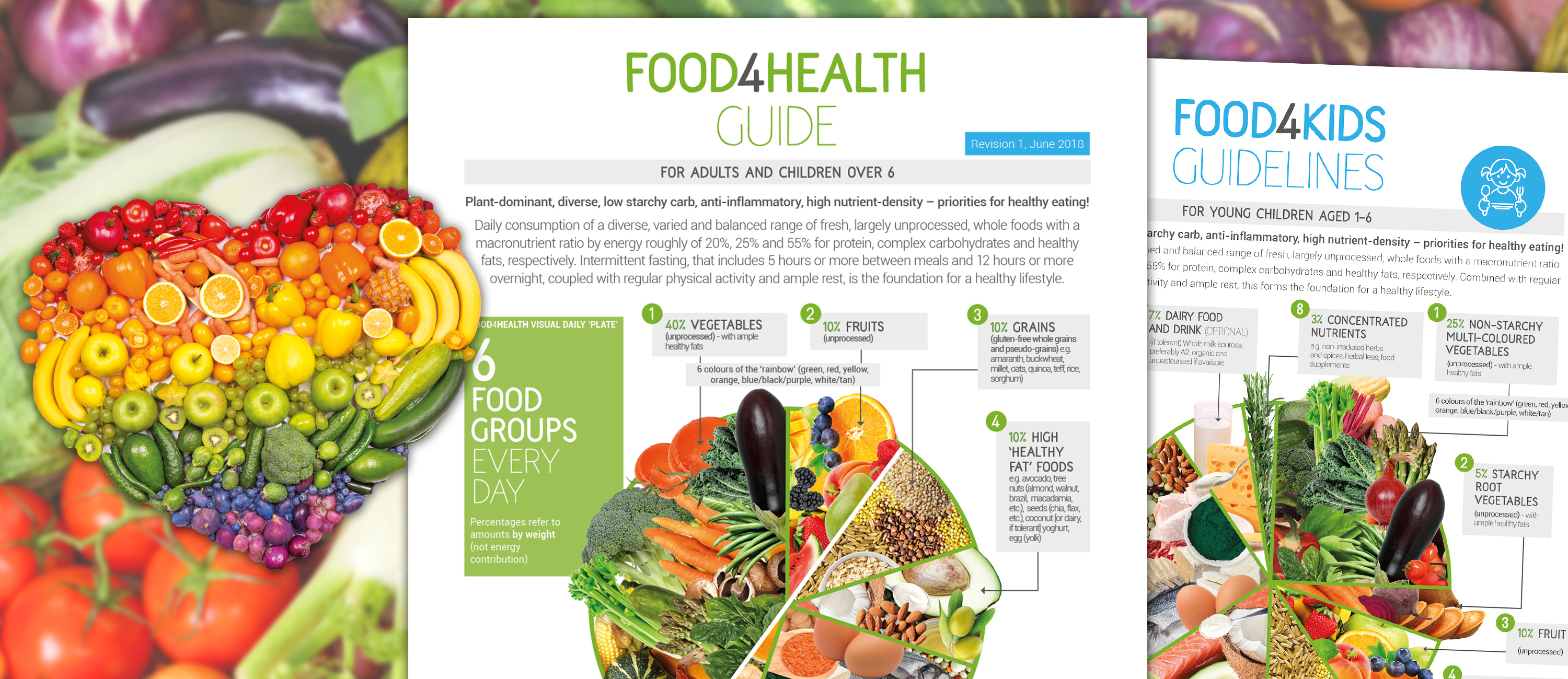
What better way to kick off our August Acceleration Series of skills, strategies and sovereignty than talking about the effect our feeding habits have on our bodies and our minds. Those of you familiar with our Food4Health campaign will know that we've been banging on for years about food being information that directs the way our genes express and not just fuel for energy.
The external challenges of the last 17 months are demanding a very high level of resilience in order to survive, but also thrive, and there is no let up on the horizon as yet. If anything, the going is going to get even tougher. It makes perfect sense then to support our bodies by recreating as much of an evolutionary feeding and fasting norm as our hunter gather ancestors. They may have faced very different challenges, but they required an equally high level of resilience in order to survive and the fact we are here, is a testament to their success.
There have been over 2,000 papers in the last ten years looking at the effects of calorie restriction on everything from single-celled organisms to primates. However, a new paper just out caught our attention, entitled, Metabolic Phenotypes and Step by Step Evolution of Type 2 Diabetes: A New Paradigm.
We think this will become a landmark paper, not only because it looks at insulin and ketones from a metabolic/hormonal signalling context, but also from an evolutionary context. There are also some groundbreaking new hypotheses that feel absolutely spot on and put pathways to actions we have instinctively known are happening. If you're new to ANH-Intl (welcome!), Rob Verkerk (our founder) and Meleni Aldridge (our executive coordinator) have been intermittent fasting and eating in a keto-adapted way for over 10 years, which is why we're so passionate about sharing the plethora of benefits.
Here's our 101 on the new paper before we talk more about the benefits of intermittent fasting - both a skill and a strategy to stand you in rock solid stead for the coming months.
How we think insulin and blood sugar are regulated
The way in which we produce and regulate insulin when we eat carbs/high sugars foods (i.e. bolus insulin regulation) is well understood.
When plasma glucose level exceeds 6 mm/L a chain reaction is set off that goes something like this:
- GLUT1 pulls in glucose into the pancreatic beta cells
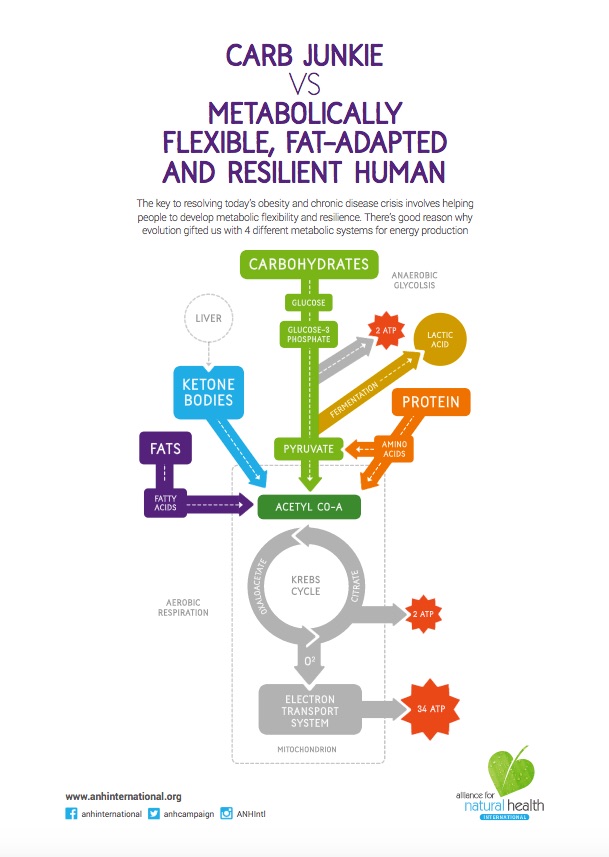
- Glucose is drawn into the mitochondria in the beta cells and there aerobic glycolysis (oxidative phosphorylation) delivers maximal ATP (adenosine triphosphate = energy) output. This ensures 36 molecules of ATP are produced for every 1 molecule of glucose, compared with just 2 molecules of ATP per molecule of glucose if the anaerobic glycolysis (fermentation) pathway was used
- This high ATP concentration closes potassium channels and opens calcium channels in the plasma membrane of the beta cells in the pancreas
- This triggers vesicles inside the beta cells containing insulin to fuse with the plasma membrane and release their contents (insulin) into the bloodstream (insulin exocytosis). This process is 2-phase (biphasic); the first phase is rapid and short-lived, and in a healthy person it’s followed by the second phase (that relies on a ‘reserve pool’ of insulin vesicles in the beta cells) that’s sustained. In type 2 diabetes (T2D), the first phase is often lost altogether and the second phase is dysregulated to a greater or lesser extent.
What we don’t understand as well is the way background levels of insulin are regulated to keep blood sugar in balance (i.e. basal glucose regulation) in the absence of carb consumption i.e. in a fasted state or on a very low carb (ketogenic) diet.
But, in essence, we know insulin is delivered in pulses every 4 (but up to 15) minutes or so and that’s controlled primarily by a hormone produced in bone cells, called osteocalcin.
In a fasted state (in a healthy person), beta hydroxybutyrate (BHB) from the liver increases and helps trigger some glucose production by the liver (gluconeogenesis) or glucose is released from stored glycogen in the liver if carbs have been consumed recently. But this isn’t enough to interfere with the all-important pulsating pattern of basal insulin secretion that underpins human evolution because our ancestors used to spend most of their time in a fasted state. This process also results in an increase of the feel-good hormone serotonin, which is known also be involved with the release (exocytosis) of insulin into the bloodstream — as well as quelling anxiety and keeping us emotionally balanced.
As someone moves down the continuum from mild blood sugar imbalance to full blown T2D, there is in fact a progression of changes in metabolism that mask the early stages of the problem. By the time it’s picked up by the HbA1c marker in a blood test or by high blood sugar (hyperglycaemia) on a reading, a person is often deep into pathology so it makes it much harder to help them reverse their disease. That’s because as insulin resistance increases, the beta cells need to produce more and more insulin to counteract the resistance (i.e. the difficulty of getting insulin into the cells where it can be used). This means that the beta cell mass in the pancreas goes up as the body tries to make more insulin to counteract the resistance in the body, which for a while cancels out or masks the problem. If nothing is done and the person keeps on exposing themselves to lots of simple refined carbs and doesn’t engage in intermittent fasting, the inability of the body to maintain this level of output and handle the ensuing free radical damage (oxidative stress) leads to the beta cells starting to die (apoptosis). This is akin - in effect - to pseudo-type 1 diabetes (T1D) and is common in later stage unmanaged or uncontrolled T2D.

Coming back to a healthy person, we know when someone’s fasted (or they’re severely restricting carbs) that the liver increases its production of the ketone BHB, a mechanism that’s controlled by the hormone glucagon (low glucagon increases ketone production). This puts a person into nutritional ketosis where the plasma BHB is maintained at low levels - generally between 0.5-3 mm/L BHB and certainly below 7 mmol/L. The medical mainstream has expressed its concern that getting people moving down the diabetic continuum to restrict carbs or fast intermittently is potentially dangerous as they could move towards diabetic ketoacidosis, which can occur when BHB goes over 25 mmol/L. However, they fail to take into account that with the steady escalation of ketones, BHB will be switched off as it's naturally regulated by insulin - even with metabolic disturbance caused by high insulin (hyperinsulinaemia) as with diabetes.
A new theory on insulin/ketone/blood sugar regulation
But here’s where the paper takes us on a significantly different journey with a new hypothesis over how insulin and glucose are regulated. Given that our natural, evolutionary state is to be fasted, the long-standing scientific view that it's insulin that controls blood-sugar can be challenged. That’s because we couldn’t afford one single high sugar meal - such as gorging on honey or fruits, something we know happened occasionally - to shut down our liver’s ability to produce glucose and so disturb our ability get glucose from the liver into cells. The normal state in the fasted, keto-adapted state is for the liver to become selectively insulin resistant so it’s not disturbed by changes in plasma insulin and can get on with its business of delivering basal, pulsed, insulin into the system.
What the researchers from Westminster University, the Mayo Clinic and the Auckland University of Technology are proposing is that the prime role of insulin is actually to regulate BHB, not blood sugar. As you restrict carbs and increase BHB, osteocalcin levels also increase. Osteocalcin then acts as the glucose uptake regulator of cells, as has long been the accepted wisdom. Osteocalcin (OCN) also triggers release of glucagon-like peptide 1 (GLP-1) which helps to force glucose uptake into cells. This process sets up a feedback mechanism that follows this sequence: BHB increase → OCN increase (+GLP-1) → insulin release → BHB decrease → OCN decrease → insulin decrease → BHB increase.
The researchers have proposed that the timing and half lives of osteocalcin and GLP-1 (half lives = 5 minutes) fit very well with the pulsative pattern of basal insulin metabolism (4 to 15 minutes), so supporting their evolutionary linkage.
What this might mean in practice
By categorising people into 3 or 4 different stages on the T2D continuum, and measuring multiple markers including blood insulin, glucose, BHB and osteocalcin, we could get a much clearer picture of where someone is in this progression, and what could help to reverse their disease or pre-clinical state.
Using HbA1c as the primary marker does nothing to help early detection of diabetes. Also the prescription of sulphonylurea and exogenous medications, like insulin, can make matters worse by creating excessively elevated blood insulin (hyperinsulinaemia) and related pathologies. Also, the complexity of the relationship between external BHB, glucagon, GLP-1 and insulin mean that the idea of simply taking exogenous ketones as supplements (or medications) might disrupt a delicate and intricate hormonal balance that has been established through millions of years of evolution.
As always, Nature knows what she’s doing. It’s just us humans that need to catch up and ‘get with Nature’s ‘program.’ Which is where calorie restriction through intermittent fasting comes in...
Calorie restriction – our evolutionary blueprint?
Despite the ongoing controversy on the specifics of the diets of our paleolithic ancestors, one thing is certain. Early Homo sapiens sapiens didn't have the luxury of kitchens with well-stocked refrigerators or the corner store at the end of the road.
Our ancestors definitely had to expend energy to feed themselves and there would have been many a lean time through the last 200,000 years. But despite the lean times, the effort required to find food and plenty of inhospitable environments, our species has survived and flourished. Therein lies a clue. Perhaps 'nature's program' factored in calorie restriction and exercise into our basic blueprint? And perhaps in doing so, turned a potential negative to a positive? It's more than interesting that, malnutrition aside, those of our species that don't have access to 'food on tap', generally live longer, healthier and happier lives. Also, they certainly don't suffer the long list of maladies common to those with well-stocked kitchens.

It's now well known that calorie restriction affects key pathways in the body that regulate metabolism, cell growth and cell proliferation. For instance, its able to deactivate the nutrient-sensing mTOR pathway, which slows down aging and prevents age-related diseases such as type II diabetes; it can also regulate insulin levels and insulin-like growth factors necessary for blood sugar control and cell growth, to name but two. When these and other metabolic pathways become disturbed, the result is, unfortunately, obesity, shorter lifespans and increased incidence of chronic disease.
Coming back to our basic blueprint as Homo sapiens sapiens, maintaining health is all about maintaining metabolic flexibility. The ability to provide sufficient energy for our bodies to perform, but not so much that we need to start storing the excess as fat and creating disease. The excess being the curse, rather than the luxury, of our modern world — the 'Well-Stocked Kitchen Syndrome'.
'Starving' intermittently for better health
Our bodies are perfectly adapted to periods of starvation and have developed a number of systems for maintaining sufficient energy for the brain, immune system and performance. In order to feed the brain during periods of starvation, the liver produces glucose from protein building blocks, amino acids, (gluconeogenesis) and ketones from fatty acids (ketogenesis). Fat cells (adipocytes) have to release the fatty acids they’re holding to fuel the ketogenesis, and, at the same time, as we've covered, secretion of insulin by the pancreas is decreased to enable the liver to carry out these specific functions.
This is why the key noticeable metabolic changes that arise from calorie restriction and intermittent fasting are gluconeogenesis (producing glucose from protein), ketogenesis (producing ketones from fatty acids), low insulin levels and increased fat-burning (lipolysis). The latter even happens in your sleep without you needing to do anything when your body has fully keto-adapted!
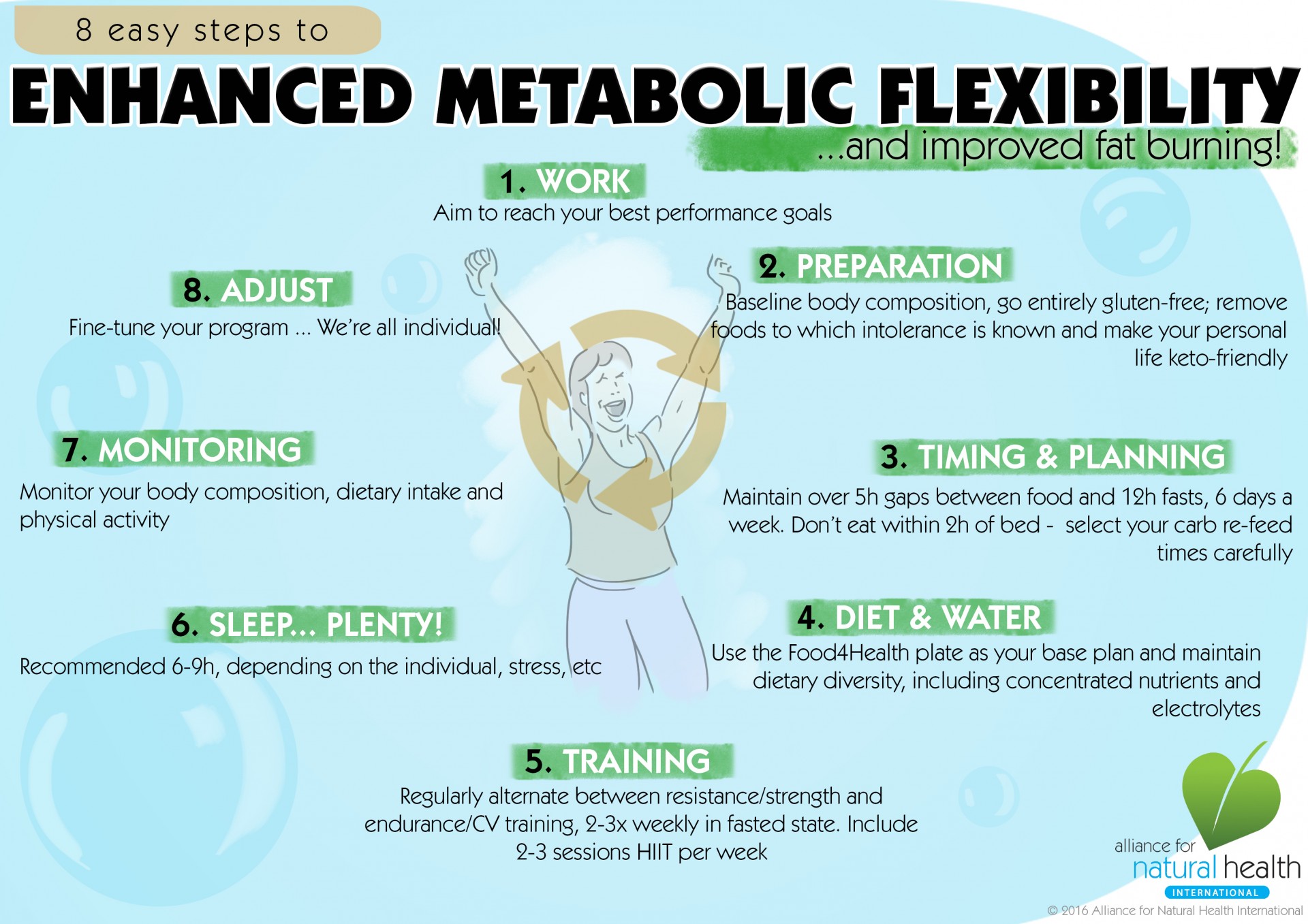
Our body has been designed to split its own proteins and fats to make energy, i.e. to be metabolically flexible naturally, rather than needing to consume huge amounts of calories for energy. Once your body has been prepared on the path of keto-adaptation, your meals are replete with dense nutrition, sufficient healthy fats and fewer starchy or refined carbs, it’s very easy and feels natural, to drop a meal so that you’re only eating two meals a day. If you fit these two meals into an 8-hour window (say between 12-noon and 8pm), you’ll be left with a 16-hour fasting window. Most people choose to drop breakfast, which is completely rational from an evolutionary perspective as we had to move and be active to find food before we could eat. Added to this, eating when your cortisol (your morning wake-up hormone) is high, becomes more of a stressor on the body than a benefit.
However, this can’t happen overnight though, and you shouldn’t expect it to. You have likely been burning sugars (from carbs) to make energy for decades, so your body will need to transition gently. Remember the old adage; 'use it before you lose it'? Well, that’s so true when it comes to our fat-burning pathways. It's the over consumption of calories (particularly empty carbohydrate calories) that disables our metabolic flexibility in the first place and hinders our fat burning potential, rendering us less resilient physically, mentally and emotionally.
Start intermittent fasting in 10 easy steps
- Take a look at what you usually eat and structure your meals around protein and vegetable carbohydrates. Limit grains to a minimum (better still cut them out!) and definitely cut out wheat and gluten-containing grains if you can. Choose organic where possible and go for grass-fed beef and wild fish and meats if you eat animal protein.
- 'Eat a rainbow' every day in terms of the colours you include from vegetables and fruits. Including a range of all the colours ensures you get a good selection of phytonutrients, which also means that your antioxidant intake will be high and help you fight free radicals.
- Don't overeat when it comes to fruit. We have no satiety system for fructose (fruit sugar) and it's very hard work for the liver to have to break it all down. Also, when the liver is busy metabolising fructose, it's not burning fat!
- Begin getting your body used to fasting by cutting out all snacks between meals and make sure you include a 5-hour fast between meals. Try and make this your new default for the future as it greatly reduces inflammation in the body.
- Start getting used to including an hour of exercise (at least 3-4 times per week) during one of your fasting periods before lunch or dinner. Ideally around 40 mins of resistance exercise (like weights) before about 20 mins of aerobic exercise (like brisk walking, running, cycling).
- Increase your activity levels so you are doing something daily – this includes walking up the stairs instead of standing on the escalators (when we can get out an about again!), gardening, cleaning the house and exercise. Remember we're programmed against inactivity, so get moving and mimic our predecessors by moving before food.
- When you feel ready – and this will differ between people depending on your metabolic flexibility – intuit which meal you’re wanting less and less and just skip it and see how you feel.
- Use exercise to release more energy when you need it. It's an interesting experience to feel hungry and instead of giving in and eating straight away, go exercise and feel your body start to provide the energy you need. It may take from a few weeks to a few months for some people to get to this point.
- When you can manage steps 7 & 8 with ease, then try fasting for 16 - 20 hours and taking your exercise before you eat your next meal. Many - me included - find this easer to do overnight, but you can still create long fasting periods if it’s lunch or dinner you prefer to skip. Once successful, repeat this process at least 3 x per month, more if you can.
- Very important: if you have health challenges then please don't undertake any radical diet and lifestyle changes without the help of your healthcare practitioner.
>>> Find out more on our Food4Health campaign page
>>> Return to Homepage








Comments
your voice counts
There are currently no comments on this post.
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences