Free speech in the Western world – especially as it relates to scientific or medical matters concerning the current pandemic has never been so threatened.
Herd immunity is the very thing we need to release us from our respective house arrests – yet we’re not being allowed to talk about it. Scientists and doctors around the world are being censored on social media unless they restrict their communications specifically to the view that vaccines are the only way that herd immunity can be achieved in relation to SARS-CoV-2.
That’s patent clap-trap and even the World Health Organization has been forced to admit that herd immunity can be achieved either by naturally-acquired infection or by vaccination (updated 31st December 2020) – it has simply indicated its preference for the latter.
In this vein, we are releasing both a video and a series of Q&As below dealing with this thorny issue. We’ve deliberately kept our discussion as uncontroversial as we can – but we felt it was imperative to communicate it because some of the principles behind it are not well understood.
We’ve initially take the punt by releasing the video on YouTube – that’s how uncontroversial we believe the information is scientifically. Politically, of course, it’s another thing – and time will tell if we need to route all views to the video via another platform.
Please share widely. We advise that you try to share this article, not only the video from YouTube, so that if we have to change the platform on which the video plays, people will still find it on our website. Thank you.
Q&A with Rob Verkerk PhD on herd immunity
1. What is herd immunity – can it only be achieved with vaccines?
To start we need to make sure we distinguish between covid-19 disease and infection by SARS-CoV-2, the virus that causes covid-19. These two things are often mixed up creating confusion for many people – including politicians. The reality is that SARS-CoV-2 is becoming more and more widely distributed, in fact it’s now almost ubiquitous having been found in waste water and sewerage systems around the world. It also shows up in hospitals where large numbers of people in the northern hemisphere tend to be very ill at this time of year and if they die and are found to also be infected with the virus their deaths are generally put down to covid-19 when, in fact, the virus may not have been the primary cause of death.
The World Health Organisation has most recently defined herd immunity in its 30th December 2020 update as follow:
'Herd immunity', also known as 'population immunity', is the indirect protection from an infectious disease that happens when a population is immune either through vaccination or immunity developed through previous infection. WHO supports achieving 'herd immunity' through vaccination, not by allowing a disease to spread through any segment of the population, as this would result in unnecessary cases and deaths.'
You’ll notice this definition recognises that herd immunity may be achieved either through naturally acquired infection or by vaccination. The reality is despite the fact that vaccination is often claimed to be the primary reason why many infectious diseases like smallpox and TB have declined the science would suggest otherwise. For as long as humans have been around naturally acquired herd immunity has always been the key process driving the interaction between human populations and the microorganisms with which we coexist of which only a tiny number cause disease and usually only in specific circumstances.
2. What makes someone more immune or more susceptible?
Everyone fits into one of three groups. Either you're part of a fully susceptible population who have no prior immunity, are highly vulnerable and this is made worse if you're also at risk of exposure to a high viral load. The second population type is those who are partially immune or tolerant. They may have had prior exposure to closely related coronaviruses such as those causing the common cold and they might have some persisting immunity from them, they may be in a lower vulnerability category and if they do get sick generally their symptoms tend to be quite mild and can easily be managed without hospital intervention. The third group are those who are fully immune. We can think of these people as being resistant to the pathogen and as more tolerant. They probably have had prior exposure to SARS-CoV-2, with the immunity that they got from that infection, that they probably didn’t even notice, and which has continued to give them immunity and they don’t have underlying vulnerabilities. Either they don’t become infected at all or they are entirely asymptomatic.
During the course of an epidemic or pandemic the relationship between these three population groups will change, with the susceptible population getting smaller. People will go down one of 3 routes: they’ll either die if they’re highly susceptible, or they might become partially immune and some, over time, can become fully immune. All of this will decrease what is known as the effective reproduction number, the R number. The most unfortunate thing is those that are most likely to die are usually both those who are most susceptible and those who are exposed to the highest viral loads, who are unable to receive the optimum treatment either in hospital settings or care homes.
Making matters even more complicated is we now have a much more complex pattern of causation, because people are not just dying of the virus. They’re dying from medical neglect, loneliness, depression, lack of purpose, a sense of isolation and many other factors that have become associated with the national and global response to the pandemic.
3. What does our immune system actually do to make us more immune?
If you’re fully immune, your body likely mounts such a strong innate immune response that virtually no virus enters your body at all and there is no significant replication of the virus in your body. You might also mount a slower slightly less competent immune response but your adaptive immune system comes to the party albeit a few days later and gets on top of the infection before it causes severe covid-19 disease.
There are a whole range of immune cells and compounds that your immune system uses to protect you from SARS-CoV-2 infection, including interferon, natural killer cells, dendritic cells, macrophages, B cells, neutralising antibodies and cytotoxic and memory T cells.
It’s important to appreciate that it is your memory T-cell immunity that gives you the longest time protection and is particularly important once your humoral immunity conferred by antibodies has subsided.
4. When does a pandemic or epidemic end? Is it something that can come back?
It’s important to appreciate that in an epidemic or pandemic, the proportion of the three populations (susceptible, partially immune and fully immune), as well as those who might die directly or indirectly as a result of the pathogen, is in a dynamic state – it’s always changing. It's most dynamic in the early stages of an epidemic. It will develop more of an equilibrium over time – but certain triggers can cause it to wax or wane. In some cases, the pathogen may more or less completely disappear – as we’ve seen with smallpox.
The point at which the epidemic starts to decline – when the effective reproduction rate is below 1, is what’s known as the herd immunity threshold.
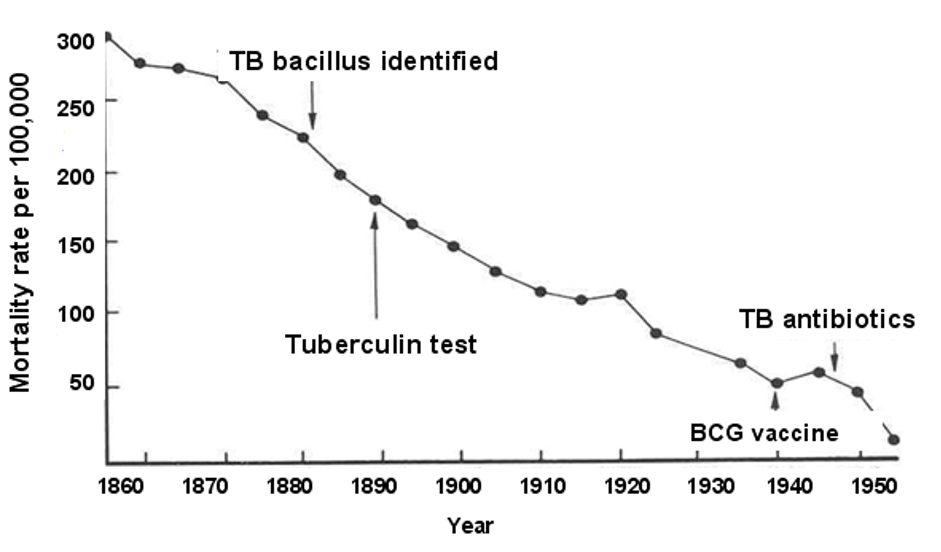
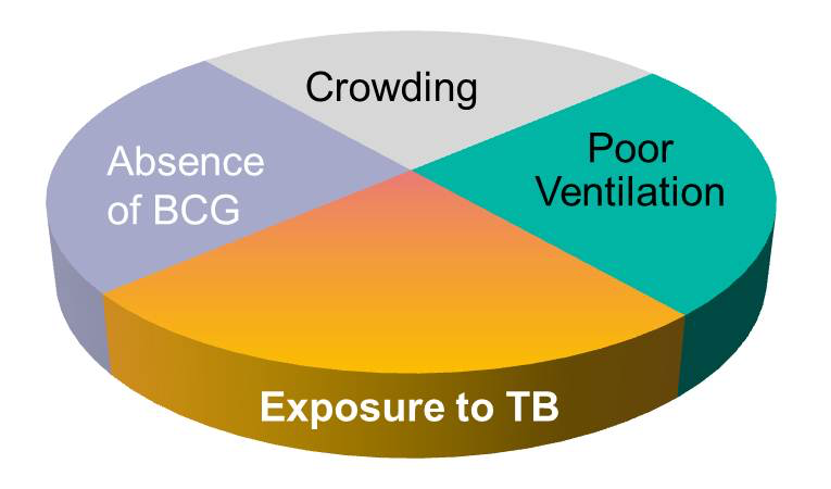
Vaccination is actually one of many components that can influence the decline of an infectious disease. This has been really well studied with many diseases and doctors and scientists at the Boston University School of Public Health have developed what they call a sufficient-cause component model that’s a useful way of looking at the problem. It has shown for example that TB related mortality was on a continuous decline in the USA from the late 19th century. Even the arrival of the BCG vaccine and TB antibiotics, both of which are often held out as being the real saviours, didn't significantly impact the general decline of the disease that is still rampant in other parts of the world, principally less developed countries.
5. How do you know when herd immunity is achieved?
The classical formula developed in the 1970s is widely used to develop the head immunity threshold.
It looks like this:
R = (1 − pC)(1 − pI)R0
Where:
- R is the effective reproduction number
- pC is the relative reduction in transmission rates due to non-pharmaceutical interventions
- pI is the proportion of immune individuals
- R0 is the basic reproduction number (i.e. fully susceptible population with no control measures)
If R is 1 or less, the HIT is said to have been met, and the epidemic will theoretically decline. Assuming an R0 of 2.0- 3.0, this formula suggests that 60-70% of the population need to be immune for the HIT to be achieved. That’s why this number gets bandied about as the target for covid vaccination programmes.
The problem with this formula is that it assumes immunity is distributed evenly through a given population and that mixing is random. It turns out both are often untrue. Also immunity to Covid-19 disease is often measured only via antibodies and not T cell reactivity so it is often under-estimated in studies. Some scientists argue that the HIT can be met when only 10-20% have effective immunity.
You can find out more about this very important area in the following articles:
- Fontanet & Cauchemez. Nat Rev Immunol 2020; 20: 583–584
- Doshi P. BMJ 2020;370:m3563
- Spelsberg A, Kiel U. BMJ 2020;370:m3563
6. What role does vaccination play?
Covid-19 vaccines either expose you to an antigen, in this case either a synthetic gene sequence that’s common to the SARS-CoV-2 virus that’s delivered inside a genetically modified, non-replicating chimpanzee common cold virus (AstraZeneca) or they make your muscle cells produce the antigen sequence having been given the instructions to do this by a synthetic messenger RNA sequence (Pfizer and Moderna).
The aim of vaccination is try to reduce the size of the susceptible population and get vaccinated people to produce an immune response that is similar to that which results following naturally-acquired infection without causing severe disease or harm
The presence of the foreign antigen sequence causes your body to mount an immune reaction, including neutralising antibodies and T cells. T cells, that provide the longest lasting immunity, as well as many other aspects of the innate and adaptive immune system which have not been studied in Phase 3 clinical trials of the emergency authorised covid vaccines. It’s also very important to remember that the ability or otherwise of vaccinated individuals to transmit virus has not been studied in these trials. The Phase 3 trials are very much still ongoing so there is still much to learn about just how safe and effective these vaccines will be for different population groups.
7. What are your most important take homes at this time?
The first thing to recognise is that vaccination is only one strategy that can help achieve the herd immunity threshold (HIT) – and that’s only if you have an effective vaccine that’s working in the real world, particularly among those who are amongst the most susceptible. The jury’s currently out on this but the data will come in over time.
Avoiding or reducing exposure to the virus (e.g. lockdowns, social distancing, masks) is only a short-term strategy and doesn’t reduce the size of the susceptible population. It also causes extensive social, economic and health disruption and damage that may exceed the benefits – which of course has been the central plank of the Great Barrington Declaration.
The herd immunity threshold is not only affected by reducing the size of the susceptible population by either letting the virus run its course or vaccination. It can also be achieved by reducing the size of the susceptible population by increasing, relatively, the size of the partially or fully immune population.
People’s susceptibility to serious disease and death can also be greatly affected by improving the protocols being delivered in hospitals. And here it’s necessary to mention the role of repurposed drugs like ivermectin – that when delivered either as prophylaxis or, often at much higher doses, for treatment with nutrients like vitamin D, vitamin C, zinc and melatonin, can deliver spectacular results – none of which are getting any airtime in the mainstream medical establishment or media. In fact there’s a proactive effort to marginalise anything that’s not vaccine related at the moment which is a travesty of good science.
>>> Review of ivermectin just published in Frontiers in Pharmacology
>>> Find out more about the I-MASK protocols by the Frontline COVID-19 Critical Care Alliance
Another really important take-home is doing what we can to reduce or eliminate vulnerability to severe disease by improving both health and nutrient status. That’s been a central plank to our sustainability blueprint and our Food4health campaigns.








Comments
your voice counts
15 January 2021 at 11:15 am
Fantastic piece; well done Rob and team. I'm genuinely fascinated that balanced perspectives like this are not discussed more widely in our communities, especially when many know about the benefits of a healthy lifestyle (optimal eating, movement and sleep). Keep them coming and I'll keep sharing!
16 January 2021 at 2:17 am
It seems that the WHO changed their definition of herd immunity in October, 2020 from the one in this article to the following:
“‘Herd immunity’, also known as ‘population immunity’, is a concept used for vaccination, in which a population can be protected from a certain virus if a threshold of vaccination is reached. Herd immunity is achieved by protecting people from a virus, not by exposing them to it.
Vaccines train our immune systems to create proteins that fight disease, known as ‘antibodies’, just as would happen when we are exposed to a disease but – crucially – vaccines work without making us sick. Vaccinated people are protected from getting the disease in question and passing it on, breaking any chains of transmission.”
Someone needs to hold them to account, it seems.
Richard.
16 January 2021 at 8:04 am
Hello Ricahrd. Yes, you're correct. The WHO did change its definition of herd immunity in October, however it then changed it again on the 31st December to the definition used in the article. Here's a link to the WHO update https://www.who.int/news-room/q-a-detail/herd-immunity-lockdowns-and-covid-19.
Warm regards
Melissa
24 January 2021 at 1:48 pm
https://www.aier.org/article/who-deletes-naturally-acquired-immunity-from-its-website/
Your voice counts
We welcome your comments and are very interested in your point of view, but we ask that you keep them relevant to the article, that they be civil and without commercial links. All comments are moderated prior to being published. We reserve the right to edit or not publish comments that we consider abusive or offensive.
There is extra content here from a third party provider. You will be unable to see this content unless you agree to allow Content Cookies. Cookie Preferences